The Future of Hand and Arm Rehabilitation
Biofeedback stands as a transformative approach, enabling individuals to consciously perceive their physiological states. Through continuous monitoring and feedback mechanisms, users develop the capacity to influence typically involuntary bodily functions such as heart rhythm, muscular tension, and cutaneous temperature. This cultivated self-awareness proves indispensable for stress and anxiety management, as people can now recognize and address physiological signals that frequently precede emotional distress.
Diverse biofeedback methodologies exist, each focusing on distinct physiological markers. Electrodermal activity (EDA) monitoring, for instance, tracks perspiration patterns, revealing valuable data about stress intensity and emotional activation. When participants receive visual or auditory cues corresponding to these physiological changes, they gradually master autonomic nervous system regulation. This acquired skill set substantially contributes to enhanced emotional stability and personal resilience.
Virtual Reality Immersion: Expanding Treatment Possibilities
Virtual reality technology introduces groundbreaking therapeutic opportunities through its immersive capabilities. By constructing lifelike digital environments, VR significantly amplifies the impact of biofeedback applications. Consider a VR simulation replicating an anxiety-provoking social scenario. Within this controlled digital space, individuals can safely practice physiological regulation techniques, subsequently transferring these skills to actual interpersonal situations.
VR's adaptive nature facilitates customized training protocols. The system dynamically modifies environmental complexity based on user performance, maintaining optimal challenge levels to sustain motivation. This tailored methodology frequently yields accelerated skill acquisition and superior therapeutic results compared to conventional approaches.
Synergistic Combination: Biofeedback Meets Virtual Reality
The integration of biofeedback with VR creates a powerful therapeutic alliance. VR's simulated environments provide risk-free arenas for practicing physiological control during stressful scenarios, while biofeedback delivers immediate performance metrics. This dual approach enables systematic development of stress management competencies through graduated exposure.
By observing physiological responses during VR sessions, users cultivate effective regulation strategies with lasting benefits. This innovative combination represents a significant advancement in addressing various mental health challenges, from everyday stress to clinical anxiety disorders.
Clinical Applications Across Multiple Domains
Beyond psychological applications, these technologies demonstrate remarkable versatility in physical rehabilitation. VR simulations enable patients to practice therapeutic movements within safe digital environments, particularly beneficial for those with mobility restrictions or recovering from injuries. When combined with biofeedback monitoring of muscular activity, treatment efficacy improves substantially, often shortening recovery timelines.
Chronic pain management represents another promising application area. VR's immersive qualities can divert attention from discomfort, while biofeedback helps patients recognize and modulate pain-related physiological patterns. This integrated strategy offers new hope for improving quality of life among chronic pain sufferers.
Ethical Considerations and Future Prospects
While therapeutic potential is considerable, implementation must address critical ethical concerns regarding data security and potential misuse. Establishing comprehensive privacy safeguards and usage guidelines remains paramount for responsible adoption. Equally important is ensuring technological accessibility through intuitive interfaces and adaptive features.
Future developments should emphasize personalized treatment algorithms and increasingly sophisticated VR environments. The continuous refinement of these technologies promises groundbreaking therapeutic innovations in coming years.
The Role of AI in Optimizing Treatment Plans
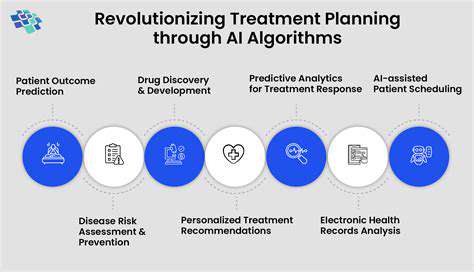
AI-Powered Treatment Planning
Artificial intelligence is fundamentally transforming treatment strategy development through data-driven personalization. Advanced algorithms process extensive patient datasets, uncovering predictive patterns that surpass traditional analytical capabilities. This enables healthcare providers to customize interventions with unprecedented precision, potentially improving success rates while minimizing adverse effects.
AI's capacity to synthesize complex medical imaging and comprehensive patient histories facilitates identification of critical success factors. The resulting personalized protocols represent a quantum leap in therapeutic effectiveness, demonstrating AI's unparalleled ability to process multidimensional variables simultaneously.
Predictive Modeling for Treatment Response
Machine learning models can forecast individual treatment responses by analyzing comprehensive medical profiles, including genetic markers and lifestyle parameters. This predictive capacity allows clinicians to prioritize interventions with optimal projected outcomes and reduced risk profiles.
Accurate response prediction revolutionizes resource allocation and treatment sequencing. By identifying probable responders early, healthcare systems can maximize therapeutic impact while conserving valuable medical resources, creating a more sustainable care model.
Personalized Treatment Recommendations
AI systems generate customized therapeutic suggestions by evaluating patient-specific data constellations. This multidimensional analysis incorporates medical background, genomic information, and behavioral patterns to produce tailored intervention strategies. Such precision medicine approaches consistently demonstrate superior clinical outcomes compared to conventional protocols.
This paradigm shift toward individualized care represents the future of medical practice. As healthcare continues evolving toward patient-centered models, AI-driven personalization will become increasingly indispensable for optimal therapeutic decision-making.
Enhanced Efficiency and Cost Savings
AI implementation generates substantial operational efficiencies throughout healthcare systems. Automated data processing and report generation liberates clinical staff for direct patient care, while optimized treatment pathways reduce unnecessary procedures and hospitalizations.
These operational improvements translate into significant cost containment without compromising care quality. The resulting economic benefits contribute to healthcare system sustainability while maintaining therapeutic standards.
Improved Patient Outcomes and Experience
The ultimate objective of AI-enhanced treatment planning focuses on superior clinical results and patient satisfaction. Precision protocols typically yield better therapeutic responses with fewer complications, significantly enhancing quality of life metrics.
By reducing trial-and-error treatment phases and accelerating positive outcomes, AI dramatically improves the patient journey. This targeted approach minimizes therapeutic uncertainty and associated stress, creating a more positive healthcare experience overall.