Pain Detection: The Hand's Defense Mechanism
Beyond Nociceptors: Other Sensory Inputs in Pain Perception
Nociceptive Input and the Context of Pain
Nociceptors represent highly specialized nerve endings that identify potentially damaging stimuli, serving as the body's frontline defense in pain detection. However, pain perception extends far beyond simple nociceptor activation, involving a sophisticated interplay of multiple sensory systems. The somatosensory system, which processes touch, temperature, and pressure sensations, actively modifies how we experience pain intensity and location. This complex integration explains why two people might report completely different pain levels from identical injuries.
Interestingly, our nervous system doesn't process pain signals in isolation. The brain constantly compares nociceptive data with information from other sensory pathways, creating what we ultimately perceive as pain. This explains phenomena like why rubbing an injured area can reduce pain perception - the additional tactile input competes with pain signals in the nervous system.
The Central Nervous System's Dynamic Role in Pain Interpretation
Our brain functions as an active interpreter rather than passive receiver of pain signals. Multiple cortical regions - including the thalamus, somatosensory cortex, and cingulate cortex - collaborate to evaluate pain signals within their broader context. This neural processing explains why identical injuries can produce vastly different pain experiences depending on circumstances, emotional state, and past experiences.
Chronic pain conditions demonstrate the CNS's plasticity in pain processing. Repeated pain signals can literally rewire neural pathways, creating hypersensitivity where even mild stimuli trigger disproportionate pain responses. This neural remodeling underscores why early, effective pain management proves crucial for preventing long-term sensitization.
Psychological Dimensions of Pain Perception
The mind-body connection manifests powerfully in pain experiences. Stress hormones like cortisol don't just affect mood - they directly increase nociceptor sensitivity throughout the body. This biological mechanism explains why periods of high stress often correlate with increased pain complaints, even without new injuries.
Cognitive factors equally influence pain perception. Attention acts as a volume control for pain signals - the more we focus on discomfort, the more intense it becomes. Conversely, absorption in engaging activities can dramatically reduce perceived pain intensity. This principle underlies many effective pain management techniques, from mindfulness meditation to immersive virtual reality therapies.
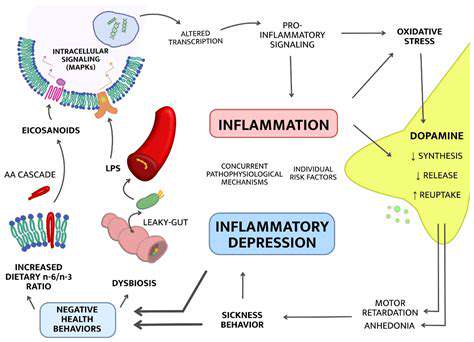
Emotional states color pain experiences profoundly. Depression doesn't just make people feel emotionally worse - it amplifies the subjective intensity of physical pain through shared neural pathways. Recognizing these psychological components enables more comprehensive, effective pain treatment approaches that address both physical and emotional aspects.
Read more about Pain Detection: The Hand's Defense Mechanism
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health