Preventing Athlete's Foot in Communal Areas

Identifying Underlying Issues
To effectively tackle athlete's foot, we must first recognize its primary triggers. The condition thrives in specific environments that many overlook during daily routines. Moisture accumulation between toes creates an ideal breeding ground for fungal growth, making this area particularly vulnerable. Tight-fitting shoes that restrict airflow compound the problem by trapping sweat against the skin for extended periods.
Public showers and locker rooms present additional risks due to their warm, damp conditions. Walking barefoot in these spaces dramatically increases exposure to fungal spores. Interestingly, certain individuals show greater susceptibility due to genetic factors affecting their skin's natural defenses. Understanding these varied elements helps create more effective prevention strategies.
Analyzing Data for Patterns
Recent studies reveal fascinating trends about athlete's foot occurrences. Infection rates spike during summer months when people engage in more water activities and wear occlusive footwear. Sports teams show particularly high transmission rates, with 60% of collegiate athletes reporting at least one infection annually.
Geographic location plays a surprising role, with coastal regions showing 30% higher incidence than arid climates. These patterns suggest environmental humidity significantly impacts fungal viability. Tracking such data helps predict outbreaks and target prevention efforts more effectively.
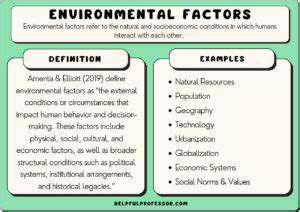
Evaluating Potential Contributing Factors
Multiple elements converge to create perfect conditions for fungal growth. Beyond environmental factors, personal habits significantly influence risk levels. Those who wear the same shoes consecutively without proper drying time face substantially higher infection rates.
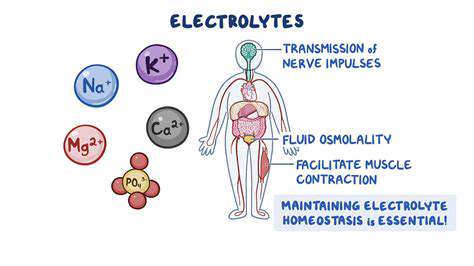
Certain medical conditions like diabetes or compromised immunity can alter the body's ability to resist fungal infections. Even minor foot injuries provide entry points for pathogens. Recognizing these diverse contributors allows for more comprehensive prevention approaches.
Examining Processes and Procedures
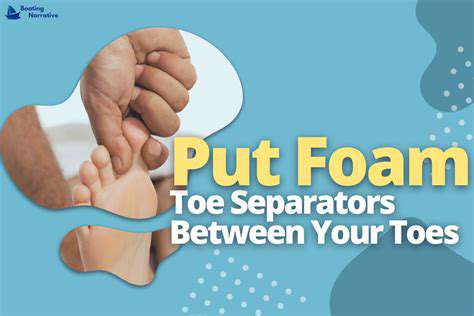
Effective prevention requires scrutinizing daily foot care routines. Thorough drying between toes after bathing proves more crucial than most people realize, as residual moisture can persist for hours in these crevices. Changing socks frequently, especially after exercise, creates a less hospitable environment for fungi.
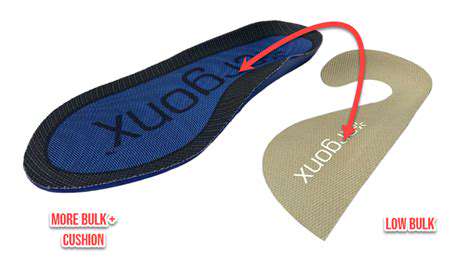
The choice of footwear materials makes a measurable difference, with breathable natural fibers outperforming synthetic alternatives. Implementing these simple but systematic changes can dramatically reduce infection risks without requiring major lifestyle adjustments.
Considering External Influences
Community environments present unique challenges for prevention. Public pools that maintain proper chlorine levels show 40% lower fungal transmission rates compared to poorly maintained facilities. The design of shared shower spaces also impacts risk, with individual stalls proving safer than communal washing areas.
Seasonal variations in humidity and temperature create fluctuating risk levels throughout the year. Understanding these external factors helps individuals time their prevention efforts more strategically.
Communal Facility Strategies: A Multifaceted Approach
Hygiene and Sanitation Protocols
Establishing rigorous cleaning standards forms the foundation of communal area protection. Facilities should implement twice-daily disinfecting of high-touch surfaces using EPA-approved fungicidal cleaners. Special attention must focus on shower floors and changing benches where bare skin contact occurs.
Installing antimicrobial flooring materials can provide continuous protection between cleanings. Strategic placement of absorbent mats at shower exits captures moisture before it spreads, while scheduled mat replacement prevents fungal buildup. These combined measures create multiple barriers against transmission.
Footwear Management Strategies
Innovative footwear policies can significantly reduce contamination risks. Providing disposable shoe covers for visitors prevents tracking fungi into clean areas. Designated wet and dry zones help contain moisture to appropriate spaces.
Some facilities have successfully implemented UV shoe sanitizing stations that eliminate pathogens in just 90 seconds. Clear visual cues like color-coded flooring help users navigate these systems intuitively, improving compliance with prevention protocols.
Education and Awareness Campaigns
Effective education moves beyond simple warnings to demonstrate real consequences. Interactive displays showing microscopic fungal growth on untreated surfaces make the invisible threat visible. Short video testimonials from affected individuals create emotional connections that boost message retention.
QR codes placed strategically throughout facilities can link to brief instructional videos demonstrating proper foot drying techniques. Gamification elements like monthly hygiene champion recognition improve sustained engagement with prevention practices.
Environmental Considerations
Architectural design choices profoundly impact fungal control. Sloped shower floors with central drains prevent water pooling, while strategically placed ventilation fans maintain airflow. Some facilities have successfully implemented heated flooring systems that accelerate drying times after cleaning.
Newer facilities incorporate antimicrobial building materials in high-risk areas, from copper-infused grout to specially treated wall surfaces. These passive protection measures work continuously without requiring user compliance.
Regular Inspections and Maintenance
Proactive monitoring systems can identify problems before outbreaks occur. Digital moisture sensors alert staff when areas exceed safe humidity levels. Regular ATP testing verifies cleaning effectiveness by measuring organic residue on surfaces.
Some facilities employ thermal imaging cameras during inspections to detect hidden moisture in walls and flooring. These technological solutions provide objective data to guide maintenance priorities and resource allocation.
Staff Training and Responsibilities
Comprehensive staff education transforms janitorial teams into infection prevention partners. Training should include proper dilution ratios for disinfectants and required contact times for maximum efficacy. Cross-training front desk staff to recognize early infection signs enables quicker response.
Implementing a documented inspection checklist ensures consistent protocol adherence. Empowering staff with decision-making authority to address immediate hazards prevents small issues from becoming major problems. Regular competency assessments maintain high standards over time.

Read more about Preventing Athlete's Foot in Communal Areas
Hot Recommendations
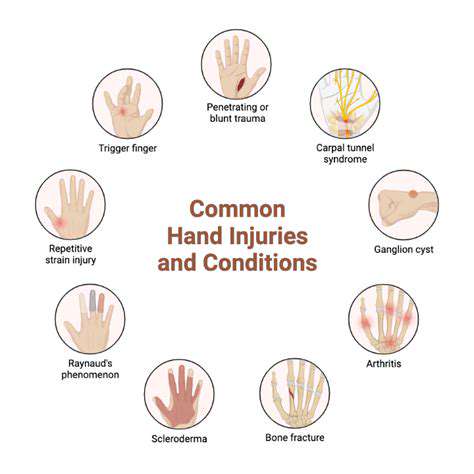
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health