The Impact of Obesity on Foot and Leg Health
The Role of Inflammation in Obesity-Related Foot Problems
Inflammation's Underlying Mechanisms
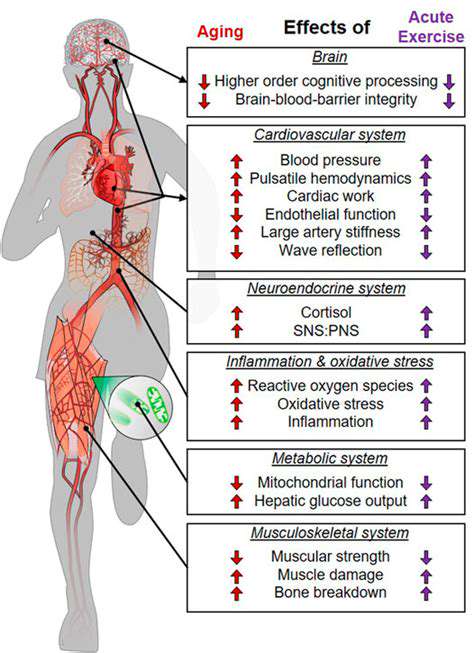
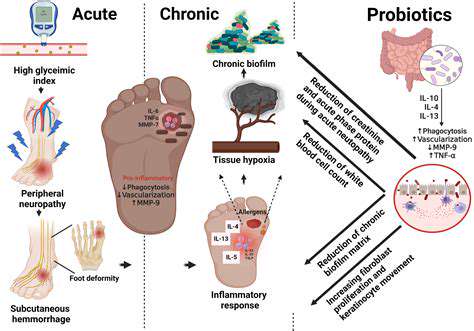
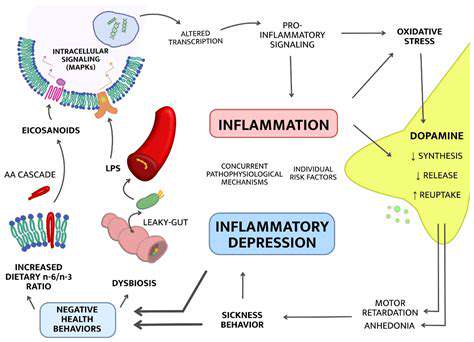
The body's defense system relies heavily on inflammation, which involves a delicate dance between immune cells and molecular signals. While acute inflammation helps fight infections and heal injuries, obesity often leads to a persistent, low-grade inflammatory state that wreaks havoc on multiple systems. This isn't your typical inflammation - it's a slow-burning fire that never fully extinguishes, constantly releasing inflammatory chemicals into the bloodstream. Over time, these inflammatory mediators like cytokines disrupt metabolic harmony, potentially triggering insulin resistance and abnormal fat deposition in various tissues.
Obesity and the Adipose Tissue Connection
Far from being inert storage, fat tissue functions as a dynamic endocrine organ pumping out hormones and inflammatory signals. As weight increases, expanding fat cells begin malfunctioning, sounding the alarm with inflammatory chemicals. The more fat someone carries, the more pro-inflammatory cytokines flood their system, creating a body-wide inflammatory environment that sets the stage for numerous obesity-related complications. Making matters worse, beneficial anti-inflammatory signals from fat tissue decrease as obesity progresses.
Consequences of Chronic Inflammation in Obesity
The constant inflammatory barrage from excess weight carries serious health consequences. Insulin sensitivity suffers first, often progressing to full-blown type 2 diabetes. Blood vessels take a beating too, with inflammation accelerating atherosclerosis and raising cardiovascular risks dramatically. The damage extends to other organs as well, contributing to fatty liver disease and even certain cancers. Grasping how inflammation and obesity feed each other is absolutely vital for creating effective prevention and treatment approaches.
Seeking Professional Guidance for Optimal Outcomes
Understanding the Root Causes of Obesity-Related Foot Problems
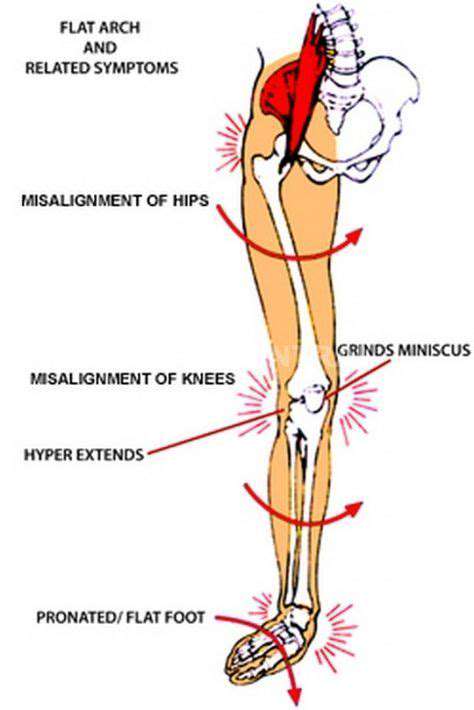
Carrying extra weight dramatically affects foot health, overloading joints, tendons and soft tissues with excessive force. This mechanical stress triggers various painful conditions while potentially limiting movement. Identifying contributing factors - from weight distribution patterns to medication side effects - proves essential for crafting personalized solutions. The additional pounds frequently worsen existing foot issues like plantar fasciitis, intensifying pain and swelling while potentially altering foot structure permanently.
Addressing the Impact of Obesity on Foot Structure and Function
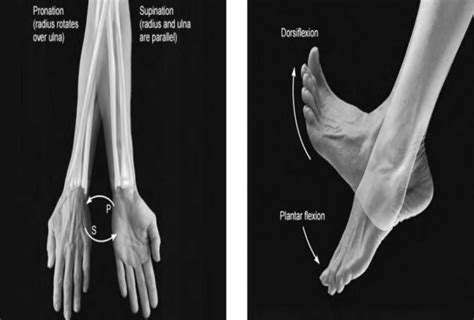
Excess weight reshapes feet fundamentally, collapsing arches under constant pressure and potentially throwing off alignment from ankles to knees. Consulting foot specialists and physical therapists becomes non-negotiable for managing these structural changes and associated discomfort. Proper footwear and custom orthotics play pivotal roles by improving weight distribution and correcting biomechanical imbalances. A comprehensive strategy addressing weight management, targeted exercises and professional foot care offers the best chance at preserving mobility and comfort.
Medical professionals provide customized weight loss plans, activity recommendations and footwear guidance tailored to individual needs. Their expertise ensures proper diagnosis and management of existing conditions while preventing new complications. This holistic approach delivers the best long-term results for maintaining foot health despite weight challenges.
Read more about The Impact of Obesity on Foot and Leg Health
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
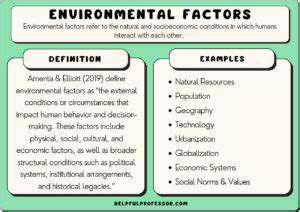
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health