The Role of Podiatrists in Maintaining Foot Health
Common Foot Conditions and Their Symptoms
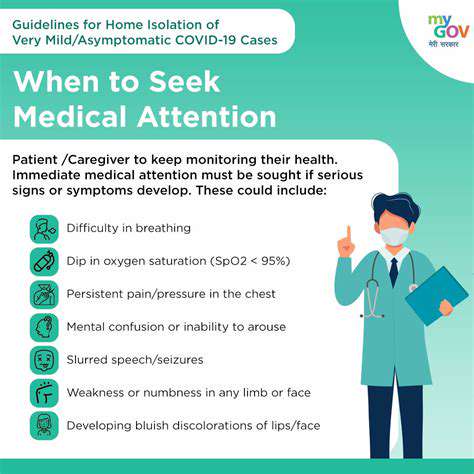
Our feet endure daily stress, making them prone to various conditions—from temporary annoyances to chronic medical concerns. Recognizing early warning signs helps prevent minor issues from escalating. Persistent discomfort, visible swelling, unusual redness, or texture changes in the skin often signal underlying problems. While online resources provide general information, nothing replaces professional evaluation when symptoms persist beyond a few days.
Joint-related conditions like arthritis frequently target the feet, causing morning stiffness and reduced mobility. Meanwhile, skin issues may develop from environmental factors or infections, requiring different intervention approaches. Monitoring your feet regularly helps catch abnormalities before they worsen—a simple habit that saves future discomfort.
Foot Pain: Causes and Management
That nagging foot pain could originate from multiple sources—acute injuries, chronic overuse, medical conditions, or simply wearing the wrong shoes all day. Effective treatment begins with identifying whether the discomfort stems from trauma, repetitive stress, or systemic health issues—each requiring distinct management strategies. A podiatrist's trained eye can discern subtle differences that self-assessment often misses.
Your shoe choices dramatically impact foot health. Well-constructed footwear acts as preventive medicine—proper arch support distributes weight evenly while adequate cushioning absorbs impact. Remember: expensive doesn't always mean better; the right fit matters more than brand names for maintaining happy feet.
Ingrown Toenails: Diagnosis and Treatment
When toenails curve into surrounding flesh, they create more than just discomfort—they open doors to infection. Catching ingrown nails early makes treatment simpler and less painful, often avoiding surgical solutions. Mild cases might respond to warm soaks and proper nail trimming techniques, while advanced cases require professional care to prevent serious complications.
Plantar Fasciitis: Understanding the Condition
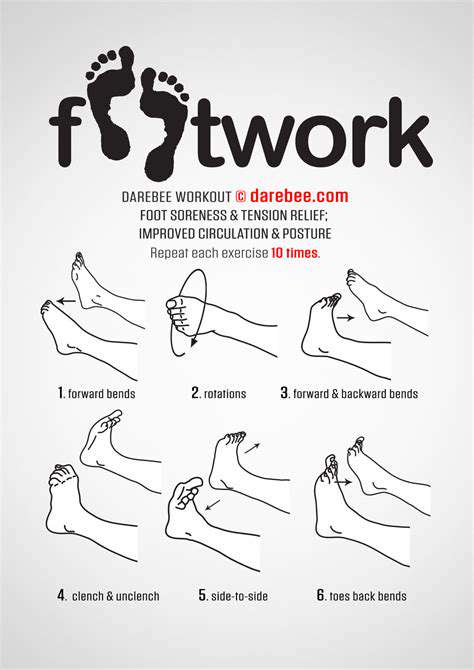
Morning heel pain that eases with movement typically points to plantar fasciitis—an overuse injury of the foot's shock-absorbing ligament. Targeted stretches combined with supportive footwear often provide more lasting relief than temporary pain medications alone. Custom orthotics sometimes become necessary for severe cases, but many patients improve significantly through consistent home exercises and activity modification.
Bunions: Causes and Prevention
Those bony protrusions at the big toe's base don't develop overnight—they grow gradually from genetic predisposition combined with footwear choices. Early-stage bunions respond well to conservative measures like toe spacers and wide shoes, while advanced cases may require surgical correction. Understanding your personal risk factors helps implement preventive strategies before noticeable deformity occurs.
Athlete's Foot: Prevention and Treatment
Contrary to its name, this fungal infection affects more than just athletes—anyone wearing damp shoes becomes vulnerable. Moisture-wicking socks and antifungal powders work better as prevention than treatment once infection sets in. While over-the-counter creams handle mild cases, persistent infections need prescription-strength medication to fully eradicate the stubborn fungi hiding in nail beds and skin folds.
The Podiatrist-Patient Partnership: Collaborative Care for Optimal Results
Understanding the Importance of Collaboration
Successful foot care resembles a dance—it requires perfect synchronization between patient and practitioner. Patients who actively engage in their treatment decisions recover faster than passive recipients of care. Meanwhile, skilled podiatrists adapt their communication style to each individual's needs—some patients want detailed explanations while others prefer concise instructions. This customized approach builds trust and commitment to treatment plans.
Effective communication flows both ways. When patients openly share their lifestyle challenges and treatment responses, podiatrists can fine-tune recommendations for real-world practicality. This dialogue transforms standard protocols into personalized roadmaps for recovery.
Active Patient Participation in Treatment
Healing isn't something done to you—it's something you participate in. Patients who take ownership of their prescribed exercises, footwear changes, and activity modifications often surprise themselves with their progress. Simple actions like keeping a symptom diary or practicing daily foot inspections provide valuable feedback for treatment adjustments.
This proactive mindset yields multiple benefits: faster symptom resolution, fewer complications, and greater confidence managing chronic conditions. When patients become true partners in care, they gain tools for lifelong foot health beyond the current treatment episode.
Tailoring Treatment Plans for Individual Needs
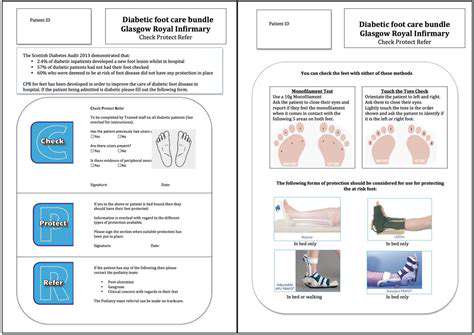
Cookie-cutter approaches fail in podiatry because no two feet—or lifestyles—are identical. A construction worker's foot injury requires different management than a ballet dancer's, just as diabetic foot care differs from sports injury recovery. The best treatment plans consider not just the diagnosis, but how the condition impacts each person's unique circumstances and goals.
Seasoned podiatrists blend clinical expertise with creative problem-solving—perhaps modifying traditional treatments or combining therapies for stubborn cases. This flexibility produces better outcomes than rigid protocols, especially for complex or chronic foot conditions requiring long-term management.
Read more about The Role of Podiatrists in Maintaining Foot Health
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health