Recognizing Symptoms of Gout in the Foot
During physical exams, doctors often look for subtle clues. The affected joint's appearance and size may vary between these conditions. Additionally, the presence of systemic inflammation or other accompanying symptoms can help differentiate them.
Role of Medical History and Physical Examination
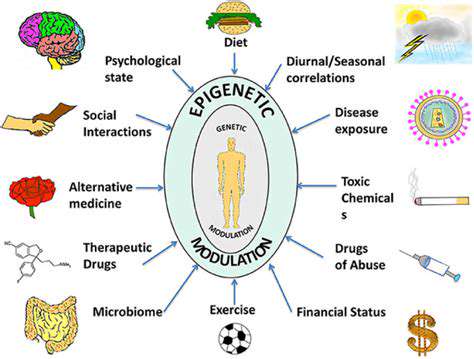
A comprehensive medical history proves invaluable in diagnosis. Details about previous joint problems, current medications, and family history of gout or similar conditions can paint a clearer diagnostic picture. This background information helps eliminate other potential causes and focuses the diagnostic process.
The physical examination provides equally crucial insights. Doctors carefully assess joint swelling, redness, and tenderness while noting any movement limitations. When combined with the patient's medical history, these observations significantly improve diagnostic accuracy.
Importance of Laboratory Tests
Confirming gout typically requires laboratory testing. Blood tests measuring urate levels often serve as the first step. While elevated uric acid levels may suggest gout, they don't conclusively prove it - additional testing remains necessary.
Joint fluid analysis offers more definitive results. Identifying needle-shaped urate crystals under microscopic examination provides unmistakable evidence of gout. This direct visualization method remains the gold standard for diagnosis.
Imaging Techniques and Their Limitations
X-rays sometimes aid diagnosis by revealing characteristic joint changes, particularly in chronic cases. However, these bone erosions aren't exclusive to gout and may appear in other conditions too.
Advanced imaging like ultrasound or MRI provides detailed soft tissue views. While helpful for assessing inflammation extent and structural abnormalities, imaging results should always be interpreted alongside other diagnostic findings.
Recognizing the Acute Gout Attack
Understanding the Initial Symptoms
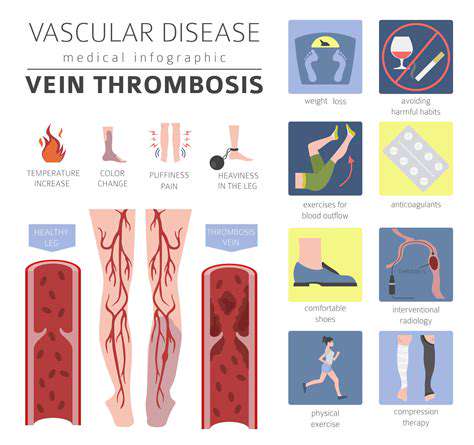
Gout attacks typically start subtly, with gradually increasing joint discomfort. Early recognition proves crucial because prompt treatment can dramatically reduce attack severity and duration. Watch for classic inflammation signs: swelling, redness, and warmth around the affected area. Many patients report these symptoms intensifying at night or after alcohol consumption or physical exertion - common gout triggers.
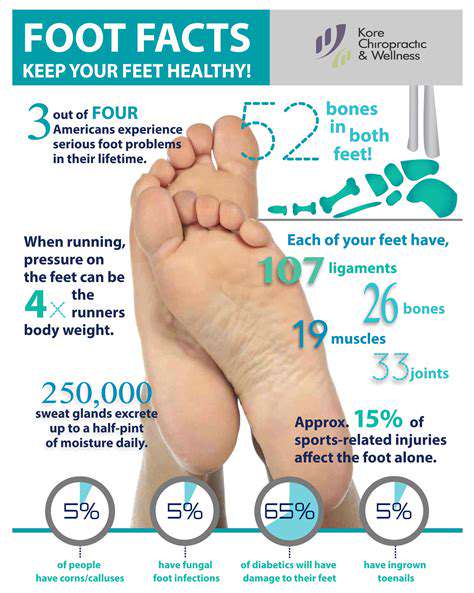
Locating the Painful Area
Gout usually causes intense pain in a single joint. While the big toe's base remains the most common site, attacks can occur in other foot joints, ankles, or knees. Precise pain location identification helps guide both diagnosis and treatment approaches.
Identifying the Redness and Swelling
Inflammation represents a hallmark gout symptom. The affected joint typically becomes red, visibly swollen, and warm to touch. These signs' intensity varies with attack severity but always indicates significant inflammatory activity.
Recognizing the Intense Pain
Gout pain is often described as among the most severe joint pains imaginable. This sharp, throbbing discomfort frequently becomes debilitating, disrupting sleep and daily activities. Such extreme pain serves as a clear warning sign requiring medical evaluation.
Considering the Timing of the Attack
Gout attacks frequently strike suddenly at night. Recognizing this pattern helps distinguish gout from other foot pains. Many patients report attacks following specific triggers like alcohol consumption, dietary excesses, or physical stress - valuable information for preventing future episodes.
Differentiating Gout from Other Foot Pains
While gout has characteristic symptoms, other conditions like arthritis, infections, or injuries can mimic them. Professional medical evaluation remains essential to ensure correct diagnosis and appropriate treatment. Proper differentiation prevents ineffective treatments and ensures optimal management of the actual condition.