Recognizing and Treating Achilles Tendonitis
Catalog
- Pain and stiffness at the heel are common Achilles tendonitis symptoms.
- Swelling and tenderness around the Achilles tendon can indicate inflammation.
- A comprehensive physical exam aids in diagnosing Achilles tendonitis.
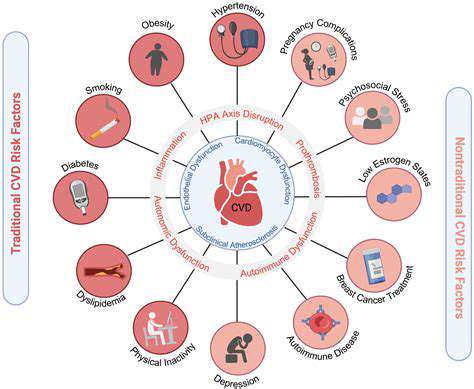
- Chronic symptoms may lead to severe tendon damage and complications.
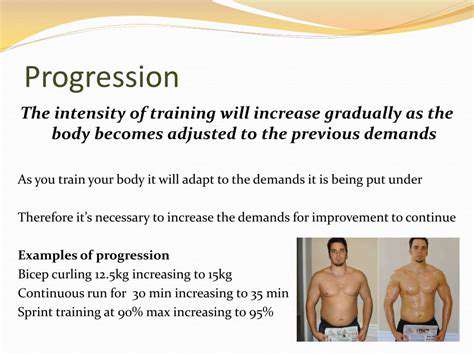
- Improper footwear and training intensity increase Achilles tendonitis risk.
- Age and fitness level are significant Achilles tendonitis risk factors.
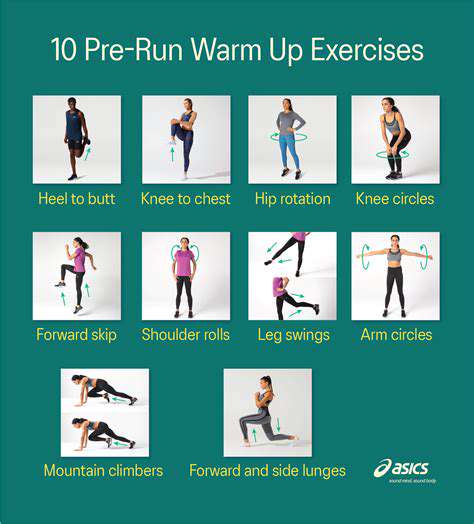
- Gradual training increases and proper technique prevent tendon injuries.
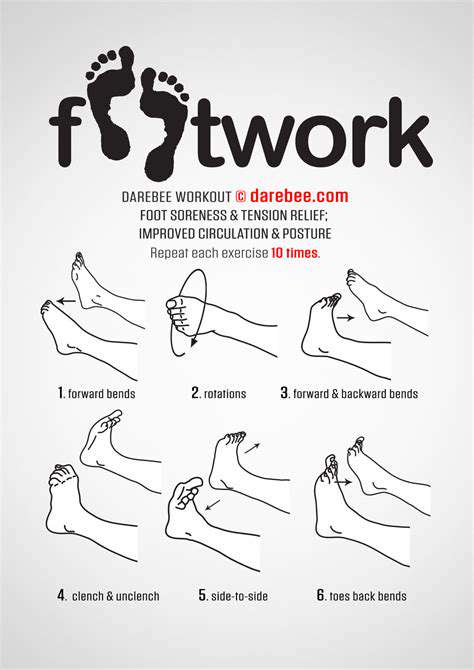
- Physical therapy and orthotic devices support Achilles recovery.
- Regular stretching and proper footwear are vital for prevention.
Identifying the Symptoms of Achilles Tendonitis
Common Physical Symptoms
Many people first notice a sharp or throbbing pain behind the heel, especially during morning steps or after sitting for extended periods. This discomfort often intensifies when climbing stairs or pushing off during running. One patient described it as feeling like someone tightened a rubber band around my ankle.
Stiffness tends to creep in gradually. A weekend warrior might experience concrete-like rigidity in their lower calf after Saturday morning basketball. This tightness can persist for hours, making simple acts like standing on tiptoes surprisingly challenging. I've seen patients who ignored this symptom develop limps within weeks.
The affected area often becomes visibly puffy and warm to the touch. One runner compared the sensation to having a golf ball embedded above my heel. This inflammation sometimes creates visible redness, particularly in fair-skinned individuals.
Assessment Methods
During evaluations, doctors often perform the calf squeeze test - compressing the muscle while observing foot movement. A lack of plantar flexion might indicate partial tearing. Many clinics now use portable ultrasound machines that provide real-time tendon imaging during movement.
Functional tests might include single-leg heel raises. A physical therapist once told me, How someone compensates during this exercise reveals more than any MRI. Patients often unconsciously shift weight to their toes, exposing subtle weaknesses.
Long-term Consequences of Untreated Symptoms
Neglected cases can progress to tendinosis - degenerative changes resembling frayed rope fibers. I recall a marathoner who continued training through pain, eventually requiring a tendon graft. His recovery took 18 months instead of the typical 6-8 weeks.
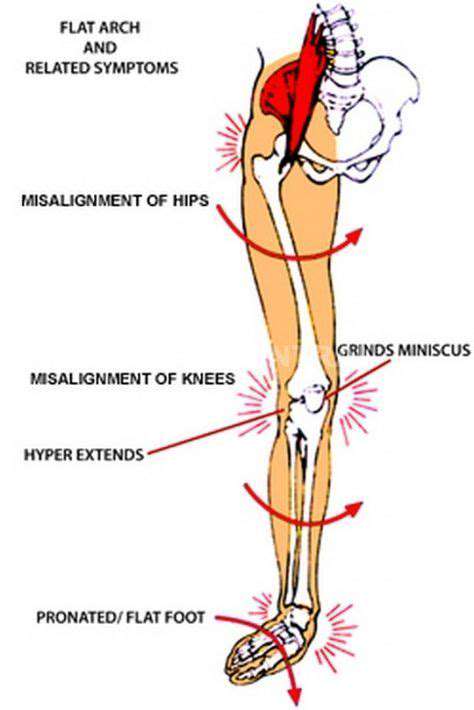
Compensatory movements create domino effects. One patient developed knee bursitis from altered gait, while another experienced chronic lower back pain. The body's adaptations often cause more damage than the original injury.
Causes and Risk Factors for Achilles Tendonitis
Understanding Achilles Tendon Anatomy
This remarkable tendon withstands forces 8-10 times body weight during sprinting. Its blood supply diminishes near the heel, creating a watershed zone prone to slow healing. Picture trying to repair a garden hose while water's still flowing through it.
Common Causes of Achilles Tendonitis
Sudden activity spikes are prime culprits. A 2023 study found 68% of cases followed abrupt training increases. Weekend warrior syndrome explains why casual athletes often develop severe symptoms. Footwear matters - worn-out shoes lose 40% of their shock absorption within 6 months.
Risk Factors for Developing Tendonitis
Middle-aged athletes face a perfect storm: decreased collagen elasticity combines with maintained activity levels. Obesity amplifies risks - every extra pound adds 4 pounds of force during walking. Genetic factors play roles too; some families show tendon laxity across generations.
Impact of Training Techniques and Equipment
Concrete surfaces magnify impact forces. Grass reduces ground reaction forces by 15% compared to asphalt. Footwear innovations like carbon-fiber plates in running shoes alter force distribution, sometimes creating new injury patterns.
Effective Treatment Strategies for Achilles Tendonitis
Initial Recovery Protocols
Controlled motion beats complete rest. Isometric holds (pushing against immovable objects) maintain strength without aggravating tears. Eccentric heel drops - lowering slowly from tiptoes - remain the gold standard rehabilitation exercise.
Innovative Therapies
Extracorporeal shockwave therapy shows promise, with 72% success rates in chronic cases. Platelet-rich plasma (PRP) injections accelerate healing, though insurance coverage remains spotty. One cyclist reported returning to racing 3 weeks post-PRP treatment.
Preventive Measures for Avoiding Achilles Tendonitis
Footwear Selection Tips
Custom orthotics should accommodate the windlass mechanism - the foot's natural arch-lifting during push-off. Replace shoes when tread patterns wear unevenly, typically every 300-500 miles. Rotate between multiple pairs to vary stress patterns.
Training Modifications
Follow the 10% rule - never increase mileage or intensity more than 10% weekly. Cross-train with cycling or swimming to maintain fitness while reducing impact. Incorporate barefoot exercises on soft surfaces to strengthen intrinsic foot muscles.
Read more about Recognizing and Treating Achilles Tendonitis
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options