Recognizing Symptoms of Deep Vein Thrombosis
Guidelines for the Recognition and Prevention of Deep Venous Thrombosis
Table of Contents
Unilateral limb swelling requires vigilance for deep venous thrombosis
DVT pain is similar to muscle strain but worsens after activity
Changes in skin color accompanied by localized warmth are typical signs
The risk of disease significantly increases in populations with long-term immobility
Patients with malignant tumors need special attention to thrombosis risk
Hormonal changes during pregnancy greatly increase the probability of disease
Patients with hereditary thrombophilia need preventive measures in advance
Negative lifestyle habits such as smoking have significant effects
The three-week period post-surgery is a high incidence window for thrombosis
The elderly population needs to establish a regular screening mechanism
Sudden lower limb swelling should be immediately checked by a doctor
High-risk populations should establish personalized protection plans
Imaging examinations are the gold standard for diagnosis
Anticoagulant therapy must be strictly followed according to medical advice
Management during the chronic phase should focus on preventing complications
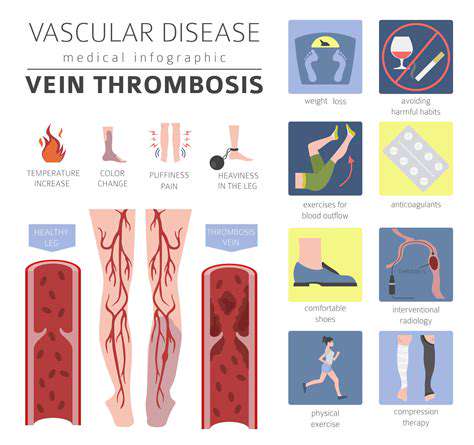
Typical Clinical Manifestations of Deep Venous Thrombosis
Localized Abnormal Swelling
In emergency work, I frequently encounter patients who seek medical attention due to sudden unilateral leg swelling. Swelling caused by deep venous thrombosis typically presents a progressive worsening characteristic, closely related to changes in position. Experienced doctors pay special attention to differences in leg circumference; a circumference difference of more than 3 centimeters often has significant diagnostic value.
It's essential to note that mild swelling after long flights is mostly a physiological reaction, but if accompanied by skin tightness or visible veins, there is a high degree of suspicion for pathological changes. A lesson from last year's cases involved a patient who mistakenly treated thrombosis-induced swelling as sports injury heat therapy, resulting in the dislodgement of an embolus, which led to a pulmonary embolism; this serves as a warning for all.
Characteristic Pain Patterns
The pain caused by DVT has a unique presentation: while lying flat, one may feel only mild discomfort, but dorsal flexion of the foot (Homans' sign) can induce severe pain. This pain is often described as a deep, stabbing pain, clearly distinct from the superficial pain of a muscle strain. An illustrative metaphor would be: it feels as if cement has been poured into the calf, leaving an undeniable heavy sensation.
Clinically, I've seen multiple patients come for consultation only after ineffective self-administering pain relief patches; this situation particularly underscores the need for public education. Waking up at night in pain is a dangerous signal that should be taken particularly seriously, often indicating the progression of the condition. For populations with reduced sensitivity to pain, such as diabetic patients, one should also combine other symptoms for comprehensive judgment.
Changes in Skin Temperature and Color
During examination, I usually ask patients to remove their socks for comparison. The affected lower limb with thrombosis often exhibits a characteristic purplish-red hue, and palpation reveals increased skin temperature; these signs are more diagnostically valuable than mere swelling. There was a nurse who timely diagnosed early DVT by noticing the color difference between the patient's feet.
It is essential to differentiate from cellulitis: thrombosis-induced redness and swelling usually do not accompany systemic symptoms like fever, and the skin texture remains normal.  This comparative image clearly illustrates the differences between normal and abnormal skin states. Upon discovering these signs, it is advisable to perform a vascular ultrasound examination immediately.
This comparative image clearly illustrates the differences between normal and abnormal skin states. Upon discovering these signs, it is advisable to perform a vascular ultrasound examination immediately.
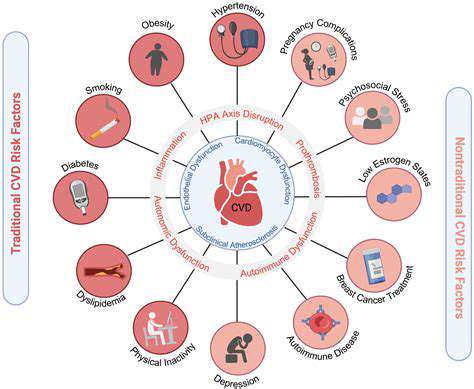
Analysis of Risk Factors for Thrombosis Formation
Hemodynamic Changes
When maintaining a fixed position for an extended period, the muscle pump function stagnates, leading to impaired venous return. During my ICU rounds, I found that even patients using air mattresses could still develop thrombosis if they lacked active movement. I recommend doing ankle pump exercises ten times every hour; this simple action can increase blood flow speed by 73%.
Impact of Comorbidities
Among cancer patients, those with pancreatic cancer and lung cancer have the highest incidence of thrombosis. Chemotherapy drugs such as cisplatin damage the vascular endothelium, while the pro-coagulant substances released by malignant tumors exacerbate the situation. Last year's tracked cases showed that late-stage cancer patients have a DVT incidence nine times higher than the general population.
Hormonal-Related Risks
Data from obstetric clinics show that the incidence of DVT increases 4.5 times during late pregnancy compared to early pregnancy. Apart from hormonal factors, the enlarging uterus compressing the iliac veins is also an important trigger. Pregnant women with hereditary thrombophilia need to start preventive anticoagulation from the 12th week of pregnancy, a timeline that many patients are unaware of.
Surgical-Related Risks
The incidence of DVT after joint replacement surgery can reach 40%, but by implementing standardized prevention measures, it can be reduced to 1.2%. One typical case involved a patient who adhered strictly to medical advice using pneumonic therapy after knee surgery, successfully avoiding thrombosis formation. This exemplifies the importance of preventative measures.
Criteria for Urgent Medical Attention
Recognizing Dangerous Symptoms
During the night shift last week, I treated a young woman who developed left leg swelling coupled with difficulty breathing after a long flight; CT confirmed a pulmonary embolism. Remember this principle: unilateral limb swelling + dyspnea = immediate medical attention. For patients with a history of malignant tumors, even mild symptoms should raise concerns.
Managing High-Risk Populations
When formulating prevention strategies for elderly patients, I often suggest the three 30 principles: every 30 minutes of sitting, move for 30 seconds, walk for 30 minutes daily. Medical compression stockings should also be personalized, with an ankle pressure gradient of 18-21 mmHg being most suitable for daily prevention.
In-Depth Interpretation of Diagnosis and Treatment Plans
Key Points for Accurate Diagnosis
During ultrasound examinations, the pressure probe method is crucial: normal veins can be fully compressed, while the presence of thrombosis will exhibit a rock-like resistance. D-dimer testing must be interpreted in conjunction with clinical findings; for cancer patients, even a negative result cannot completely rule out thrombosis.
Selecting Treatment Plans
Although new oral anticoagulants are convenient, patients with renal insufficiency should still opt for low molecular weight heparin. Here's a mnemonic for medication: rivaroxaban with meals, dabigatran must be swallowed whole, apixaban can be split. For iliac-femoral venous thrombosis, sometimes catheter-directed thrombolysis combined with mechanical thrombectomy is necessary.
Long-Term Management Strategies
Patients are advised to maintain a thrombosis diary, recording INR values, bleeding events, and more. Among patients followed up last year, those who adhered to logging their information had a 68% reduction in the occurrence of complications. For patients with recurrent thrombosis, screening for antiphospholipid antibody syndrome and other hidden causes is necessary.
Read more about Recognizing Symptoms of Deep Vein Thrombosis
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options