How Hand Pain Can Indicate Underlying Health Issues
Contents
Repetitive motion injuries contribute significantly to hand pain in workers.
Health conditions like arthritis can cause joint pain and discomfort in hands.
Accidents leading to fractures or sprains result in immediate hand pain.
Age can bring wear and tear, affecting joint health and causing hand pain.
Autoimmune disorders often lead to chronic hand pain and symptoms like swelling.
Hand pain may indicate cardiovascular issues, necessitating prompt medical evaluation.
Neurological conditions like carpal tunnel syndrome result in pain and numbness.
Recognizing warning signs of hand pain can lead to timely medical intervention.
Discussing symptoms effectively can improve diagnosis and treatment outcomes.
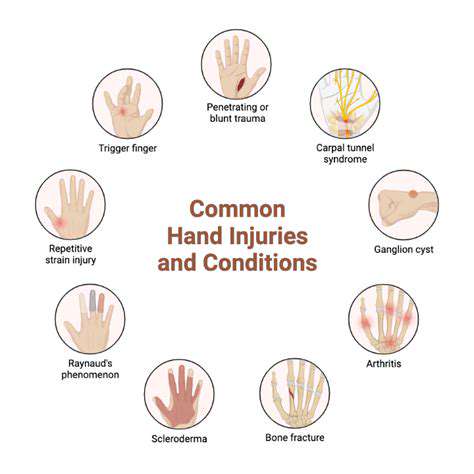
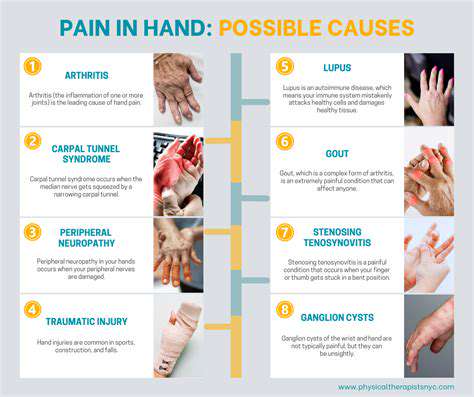
Common Causes of Hand Pain
Work-Related Injuries
Many individuals experience hand pain due to repetitive motions or strain from their jobs.
- Repetitive motion injuries
- Forceful exertions
- Workplace ergonomics
Additionally, forceful exertions during tasks can lead to muscle fatigue and cumulative damage over time. Consider adjusting your workspace to enhance comfort and efficiency, which can significantly lower the risk of injury.
Health Conditions Related to Hand Pain
Several underlying health issues can manifest as Hand Pain, including arthritis and diabetes. According to the Arthritis Foundation, about 54 million adults in the United States have some form of arthritis, leading to joint pain and inflammation that often affects the hands. Awareness of the symptoms can facilitate early intervention.
Diabetic neuropathy is another condition that can lead to pain and numbness in the hands. It's essential for those with diabetes to monitor their blood sugar levels regularly, as fluctuating glucose can exacerbate nerve-related pain.
Injuries from Accidents or Falls
Accidents, such as falls or impacts, can cause immediate and severe hand pain. Fractures or sprains resulting from these accidents often exhibit symptoms like swelling and bruising. Adhering to safety protocols in work and home environments can help mitigate the risk of these injuries.
For people involved in sports or physical activities, proper techniques and equipment can further prevent injuries. If you suspect a fracture, seeking immediate medical attention is vital to avoid long-term complications.
Age-Related Wear and Tear
As we age, it's common for wear and tear to affect our joint function and overall hand health. Conditions like osteoarthritis often develop gradually and can lead to noticeable discomfort. Epidemiological studies show that nearly 27 million Americans over the age of 25 are affected by osteoarthritis, primarily in the hands.
It's vital to engage in regular physical activity that emphasizes flexibility and strength training for the hands. Such preventative measures can help maintain mobility and slow down the progression of age-related joint issues.
Link Between Hand Pain and Autoimmune Disorders

Understanding Autoimmune Disorders
Autoimmune Disorders occur when the immune system erroneously attacks healthy cells, mistaking them for foreign invaders. This miscommunication can lead to chronic inflammation and significant tissue damage. Conditions like rheumatoid arthritis, lupus, and Sjögren's syndrome represent major types of autoimmune diseases that often affect the joints and can manifest through persistent hand pain and swelling.
Recent studies suggest that approximately 24 million people in the U.S. suffer from autoimmune disorders, with hand pain being one of the key symptoms. This highlights the importance of early diagnosis and proper management to prevent further complications associated with these conditions.
Symptoms of Hand Pain in Autoimmune Disorders
- Joint stiffness and swelling
- Reduced range of motion
- Numbness or tingling sensations
- Fatigue and generalized malaise
Hand pain related to autoimmune disorders often presents through a variety of symptoms that can vary significantly from person to person. Persistent joint stiffness, especially upon waking, is particularly common and can render simple tasks like typing or holding objects painful. This discomfort can also be accompanied by swelling and redness, indicating active inflammation in the affected joints.
Diagnosing Autoimmune Disorders
Diagnosis typically begins with a thorough medical history and physical examination to assess joint health and pain levels. Physicians may employ blood tests to detect specific autoantibodies, inflammatory markers, and other indicators of autoimmune activity, including rheumatoid factor and anti-CCP antibodies. As a part of comprehensive diagnostics, imaging tests like X-rays or MRIs may be used to visualize joint damage.
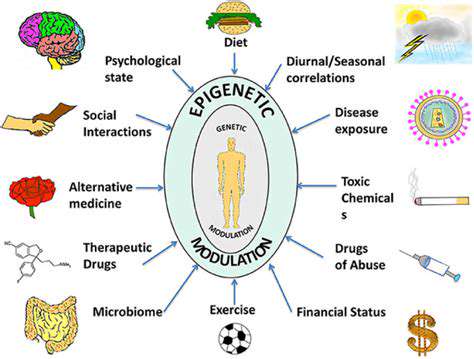
Impact of Lifestyle Factors
Lifestyle choices play a crucial role in both the progression of autoimmune diseases and the management of related hand pain. Diet, exercise, and stress management can substantially affect inflammation levels in the body. Nutrient-rich foods, such as fruits, vegetables, and omega-3 fatty acids, have shown promise in reducing inflammation. Regular low-impact exercises aid in maintaining joint function and can relieve stiffness.
Additionally, mindfulness practices and stress reduction techniques can support mental health, which is often challenged by chronic pain. Patients should consider a holistic approach when managing symptoms of autoimmune disorders.
Potential Treatments for Hand Pain
Treating hand pain associated with autoimmune disorders often involves a multi-faceted approach. NSAIDs (nonsteroidal anti-inflammatory drugs) and corticosteroids are commonly prescribed to manage inflammation and pain. In some cases, disease-modifying antirheumatic drugs (DMARDs) may be used to change the course of the disease itself, potentially reducing long-term joint damage.
Physical therapy can also play a pivotal role in recovery. Strengthening exercises can help improve mobility and function in the hands, reducing pain over time. Additionally, occupational therapy can teach patients how to modify daily activities to minimize strain on affected joints.
Prevention and Management Strategies
While there is no guaranteed way to prevent autoimmune disorders, early detection and lifestyle modifications can significantly improve patient outcomes. Maintaining a healthy diet, engaging in regular physical activity, and avoiding known triggers can be effective strategies. Regular check-ups with healthcare providers are crucial to monitor any changes in symptoms and adapt treatment plans as necessary.
Establishing a support network can provide both emotional and practical help, enabling individuals to better cope with their condition. Encouragement from peers and professionals can make a significant difference in the overall management of autoimmune diseases.
Future Research Directions
Ongoing research into the pathophysiology of autoimmune disorders is paving the way for novel therapeutic approaches. Currently, investigations into biotherapies, personalized medicine, and regenerative treatments offer promising avenues for future application. These advancements could lead to more effective interventions with fewer side effects, improving quality of life for many individuals suffering from hand pain related to autoimmune diseases.
The rapid pace of biotechnological innovation means that patients should remain informed about new treatment options as they become available. Staying engaged with the latest research can empower patients to make informed decisions about their health and treatment journeys.
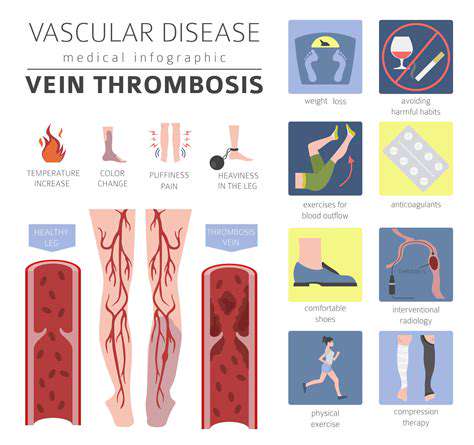
Cardiovascular Health and Hand Pain
Understanding the Connection Between Hand Pain and Cardiovascular Disease
Research has shown that hand pain can sometimes be a symptom of Cardiovascular Diseases, particularly when linked to conditions like peripheral artery disease (PAD). PAD occurs when there is reduced blood flow to the limbs, often due to plaque buildup in the arteries. In such cases, patients may experience pain or cramping in their hands during physical activity, which can be a warning sign that should not be ignored. A medical assessment is critical to determine the underlying cause.
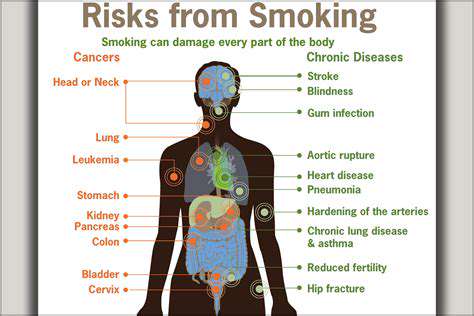
Moreover, studies indicate that the presence of hand pain may coincide with other cardiovascular risk factors, such as high blood pressure, high cholesterol, and diabetes. Understanding this linkage is crucial for ensuring early interventions can be undertaken. Because many individuals may dismiss pain in their hands as a mere byproduct of age or overuse, raising awareness about this connection is essential for proactive healthcare.
The Impact of Peripheral Artery Disease on Daily Life
Living with peripheral artery disease (PAD) can significantly alter day-to-day activities, especially tasks that require the use of hands. Individuals might find that their grip strength decreases or that activities like typing or holding objects become challenging due to discomfort. This not only affects personal productivity but can also have social repercussions, as it limits engagement in hobbies or interactions that require fine motor skills.
Regular monitoring and consistent management of PAD can enhance quality of life. For instance, a structured exercise ritual, along with dietary adjustments aimed at improving overall vascular health, can provide relief. Patients should also work closely with healthcare providers to manage risk factors effectively, as this proactive approach can mitigate symptoms of hand pain while improving overall cardiovascular health.
Preventive Measures for Maintaining Hand Health and Cardiovascular Wellness
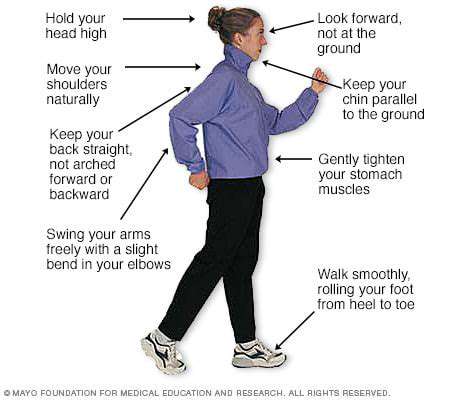
Preventing diseases such as PAD and managing hand pain involves a multifaceted approach. First and foremost, maintaining a balanced diet rich in fruits, vegetables, and whole grains can help control cholesterol levels and blood pressure. Regular physical activity tailored to individual capabilities is equally crucial, as it promotes better circulation and muscular strength, reducing the likelihood of developing severe symptoms.
Additionally, practices such as quitting smoking are fundamental, as tobacco use considerably exacerbates the risk of cardiovascular illnesses. Staying hydrated and practicing ergonomic techniques while engaging in repetitive hand motions can also alleviate unnecessary strain and reduce the risk of injury. More than anything, fostering a comprehensive routine that addresses both cardiovascular health and hand functionality is vital for long-term wellness.
When to Seek Medical Attention for Hand Pain
Recognizing when to seek medical attention for hand pain is vital, particularly as it may indicate underlying cardiovascular issues. Individuals experiencing persistent pain, changes in skin color, or reduced temperature in their hands should consult a physician immediately. It’s essential to provide healthcare professionals with a thorough history of symptoms, lifestyle habits, and any family history of cardiovascular conditions.
In conclusion, early detection can lead to more effective management of both hand pain and cardiovascular health. Collaboration with healthcare practitioners can also lead to tailored strategies for pain management that can improve quality of life. Staying informed about the possible connections between seemingly isolated symptoms is crucial for overall health and well-being.
Neurological Conditions Associated with Hand Pain
Common Neurological Conditions That Cause Hand Pain
- Carpal Tunnel Syndrome - a common condition causing pain and numbness in the hand.
- Peripheral Neuropathy - affects peripheral nerves, often leading to burning or tingling sensations.
- Radiculopathy - results from nerve root compression in the spine, affecting hand function.
- Multiple Sclerosis - a progressive disease potentially leading to hand weakness and coordination issues.
One of the most prevalent neurological conditions associated with hand pain is Carpal Tunnel Syndrome (CTS). This condition occurs when the median nerve, which runs through the wrist, gets compressed. Symptoms include numbness, tingling, and weakness in the hand, especially noticeable when performing tasks such as typing or holding objects. Recent studies indicate that approximately 3-6% of the adult population is affected by CTS, with women being three times more likely to experience it than men.
Another significant condition is Peripheral Neuropathy, which can result from various factors including diabetes, trauma, or infections. Patients with neuropathy often describe symptoms as burning or tingling sensations in their hands and feet. According to the American Academy of Neurology, nearly 30% of diabetes patients develop some form of neuropathy, making awareness and management crucial.
Symptoms and Diagnostic Approaches for Neurological Hand Pain
Diagnosing neurological conditions related to hand pain begins with a thorough medical history and physical examination. Physicians often use specific tests to determine the underlying causes of symptoms, which might include electromyography (EMG) or nerve conduction studies. These tests can reveal how well the nerves are functioning and whether any damage is present. If a doctor suspects conditions like radiculopathy or neuropathy, imaging studies may also be utilized to assess underlying spinal problems.
Patients often present a variety of symptoms. For example, pain could come along with weakness, numbness, and reduced grip strength, widely varying among individuals. Recognizing these symptoms early can help in the timely management of underlying conditions. Therefore, if someone experiences persistent or escalating hand pain, seeking an assessment from a healthcare professional is essential. Notably, early intervention can significantly enhance treatment outcomes and eventually improve quality of life.
When to Seek Medical Advice
Recognizing Warning Signs
Hand pain can manifest in various ways, ranging from sharp pain to a dull ache. It’s essential to pay attention to the type and intensity of the pain, as well as any accompanying symptoms. For instance, consistent tingling or numbness could indicate nerve compression, while swelling or redness may suggest an inflammatory condition. The American Academy of Orthopaedic Surgeons advises individuals to monitor these signs closely, as they can provide critical clues about underlying health issues.
If you experience persistent pain, it may be time to consult a healthcare professional. Delaying a visit could worsen potential conditions like arthritis or carpal tunnel syndrome. It's important to remember that early diagnosis often leads to better treatment outcomes and can prevent more severe complications down the line.
Timing Your Consultation
Determining when to Seek medical advice can sometimes be challenging. A good rule of thumb is to schedule an appointment if your hand pain lasts more than a week without improvement. Additionally, if the pain interferes with daily activities, such as writing or gripping objects, it’s a definite sign that you should consider professional advice. The Centers for Disease Control and Prevention (CDC) notes that early intervention can often mitigate more serious health problems.
Specific Conditions to Consider
Hand pain doesn't occur in isolation; it can often signal various medical conditions that require attention. For instance, conditions such as rheumatoid arthritis present with joint pain and stiffness, particularly in the mornings. Tendonitis, often seen in athletes or those who perform repetitive tasks, also leads to significant discomfort. A healthcare provider can conduct thorough examinations, including imaging tests, to identify these specific issues and recommend appropriate treatment options.
Moreover, it's prudent to consider non-physical causes of hand pain, such as systemic diseases like diabetes or thyroid dysfunction. These conditions can lead to neuropathy, which manifests as pain or other sensations in the hands. A comprehensive assessment of your health can ensure that these underlying issues are not overlooked.
Discussing Your Symptoms Effectively
When visiting a healthcare professional, being able to clearly articulate your symptoms can lead to a more accurate diagnosis. Take note of when your pain occurs, any triggers you’ve identified, and the duration and intensity of the discomfort. Prepare to discuss your medical history and any lifestyle factors that might contribute to your hand pain. Effective communication can significantly enhance the quality of your visit and help your doctor make informed decisions.
Additionally, don't hesitate to list any treatments you've already tried. Understanding what has or hasn’t worked can provide your doctor with important insight. Being proactive in your communication helps create a productive environment for addressing your hand pain and ensures you feel respected and involved in your treatment plan.
Read more about How Hand Pain Can Indicate Underlying Health Issues
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options