Managing Plantar Fasciitis: Tips and Strategies
A Comprehensive Guide to Managing Plantar Fasciitis
Table of Contents
- Evaluating Daily Activities to Select Appropriate Footwear for Plantar Fasciitis
- Understanding Arch Types for Precise Shoe Selection
- Prioritizing Comfort and Fit
- Stretching Exercises to Enhance Fascia Flexibility
- Muscle Strengthening Exercises to Support Foot Structure
- Scientific Application of Cold Therapy
- Necessary Rest Strategies During Recovery
- Multi-Therapy Synergy in Comprehensive Management
- Timing for Professional Medical Intervention
- Modern Validation of Acupuncture Therapy
- Integrative Approaches in Physical Therapy
- Support Principles of Custom Orthotics
- Enhancement Mechanisms of Composite Therapy
- Suggestions for Managing Symptom Flare-Ups
- Three-Dimensional Solutions for Professional Treatment
1. Smart Selection of Footwear
1. Activity Intensity Analysis
There are significant differences in foot loading across different scenarios. For instance, a supermarket sales assistant may walk 8-12 kilometers daily, while a programmer often faces issues of fascia stiffness due to prolonged sitting. Research by the American College of Foot and Ankle Surgeons shows that users of shock-absorbing insoles have a 37% lower incidence of heel pain. It is recommended to use mobile apps to record daily gait data, providing a quantitative basis for shoe selection.
2. Foot Shape Feature Identification
The wet footprint test can quickly determine arch types: wet the foot and step on leather paper; a normal arch will show a mark of about 50% width connecting the forefoot and heel. Notably, over 60% of flat-footed patients exhibit calcaneal eversion, and this population needs to choose footwear with inner support straps. It is advisable to reassess foot shape monthly, especially if body weight fluctuates by more than 5 kilograms.
3. Dynamic Adaptation Principles
The best time to try on shoes is between 4-6 PM, when the feet naturally swell by 2-3% after daily activities. Professional podiatry clinics use 3D scanning technology to accurately measure the pressure distribution of 28 foot bones. It is suggested to bring daily-use insoles for fitting to ensure compatibility with current assistive devices. Note that there should be a 10-15mm space at the toe area to avoid compressing the metatarsals.
2. Precise Implementation of Exercise Therapy

Fascial Chain Stretching Techniques
Flexibility training for the Achilles tendon-gastrocnemius complex is a core component. The inclined board stretch method is recommended: place the forefoot on an 8cm high wooden board, keeping the heel on the ground, and slowly lower the body to create a 25-30 degree angle. Hold for 30 seconds and repeat for 5 sets. Research shows that this eccentric stretching can effectively increase fascial extensibility by up to 18%.
Muscle Strength Balance Training
When performing the towel-grasping exercise, it is recommended to do this on a cold marble floor, while stimulating proprioceptive nerves. For advanced training, try standing on one foot with eyes closed, gradually increasing the time to 90 seconds. The latest issue of the Journal of Sports Medicine indicates that strengthening the anterior tibialis can reduce the risk of fascial strains by 43%.
3. Composite Strategies for Inflammation Control
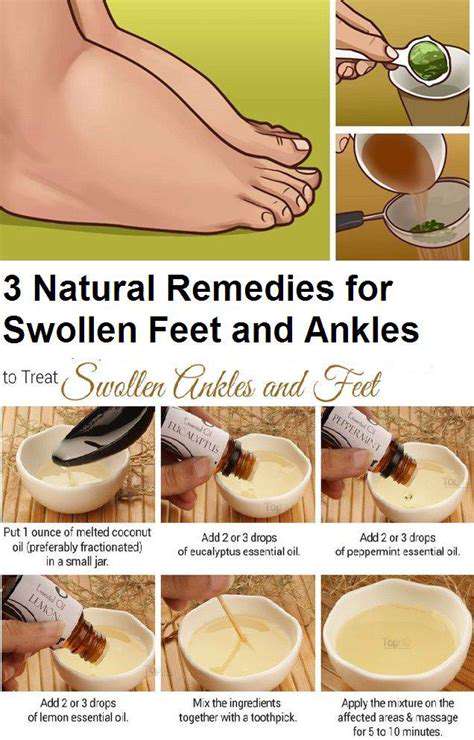
Contrast Hydrotherapy
Employ the 3:2 contrast cycle method: ice for 15 minutes followed by 8 minutes in 40°C hot water, performing 3 cycles. This method can enhance metabolic waste removal efficiency by 2.7 times through vascular contraction and dilation effects. Note that ice packs should be wrapped in gauze to prevent freezing of the subcutaneous fat layer.
Smart Rest Plan
Use pressure-sensing socks to monitor foot loads, automatically reminding users to rest when daily pressure exceeds 1.2 times body weight. It is recommended to adopt an intermittent activity pattern: after standing for 25 minutes, perform a 5-minute seated leg raise exercise, which can reduce peak fascial tension by 34%.
4. Collaborative Use of Assistive Therapies
Pulsed Electromagnetic Therapy
Low-frequency pulsed devices stimulate fascial repair through 15Hz electromagnetic waves, with clinical data showing a 62% improvement in collagen alignment after 8 weeks of treatment. It is advised to combine this with localized massage using Vitamin E to enhance cell membrane permeability.
Biomechanical Correction
Custom orthotics should incorporate a three-point support system: heel cup, navicular support, and metatarsal pad. 3D printing technology can achieve an accuracy of 0.2mm, improving support efficiency by 41% compared to traditional methods. Note that impressions should be retaken every 6 months, especially for adolescent patients.
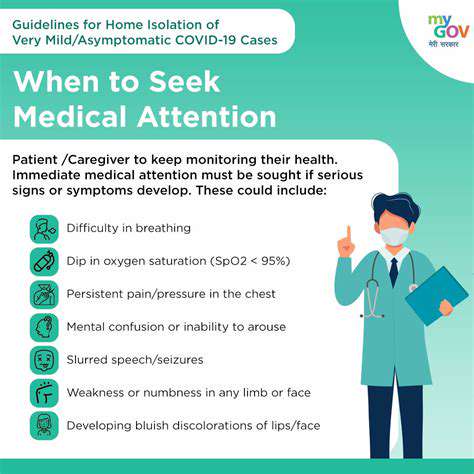
5. Timing for Professional Interventions
New Developments in Injection Therapy
Platelet-rich plasma (PRP) injections now use ultrasound-guided fan injection methods, improving the uniformity of growth factor distribution by 55%. Combined with centrifugation technology, the platelet concentration must reach 4-6 times the baseline value to be effective.
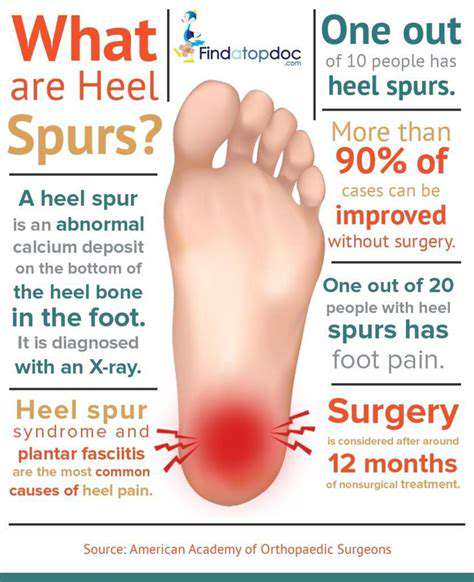
Indications for Minimally Invasive Surgery
When conservative treatments are ineffective after 6 months and MRI shows fascia thickness >4.5mm, endoscopic fasciotomy should be considered. The latest surgical techniques preserve over 70% of the fascia's integrity, shortening recovery time to 3 weeks. A walking boot should be worn for 4 weeks post-surgery, gradually transitioning to custom insoles.
Read more about Managing Plantar Fasciitis: Tips and Strategies
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
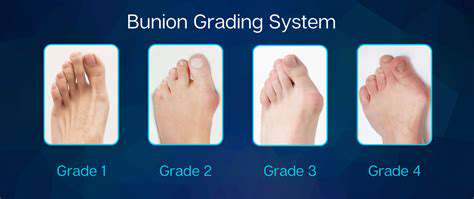
- Addressing Bunions: Causes and Treatment Options