Identifying Symptoms of Stress Fractures in the Foot
Catalog
- Localized pain during exercise may indicate a stress fracture
- Swelling and tenderness often accompany stress fracture symptoms
- Bruising may suggest the need for professional medical evaluation
- Altered gait often reflects underlying foot issues
- Unexplained fatigue may be related to skeletal injuries
- Imaging studies are key tools for diagnosis
- Early detection can enhance recovery efficiency
- Ignoring symptoms may lead to chronic pain
- Ongoing discomfort requires timely medical attention
- The RICE principle promotes injury repair
- Nutritional intake affects bone strength
- Training methods determine injury risk
- Shoe selection impacts protective effectiveness
This article analyzes the identification and response strategies for stress fractures in the foot.
Common Symptoms of Stress Fractures in the Foot

Pain Characteristics Identification
Sharp pain in specific areas of the foot during weight-bearing should raise concerns. This discomfort typically presents as intermittent dull pain in the early stages of exercise, potentially developing into persistent pain as activities continue. A marathon runner once described: 'Every time the sole of my foot touches the ground, it feels like the third metatarsal is being hit with a hammer,' this vivid description illustrates the issue well. It is advisable to record the frequency and intensity of pain episodes, as plotting symptom variation can assist doctors in making judgments.
Swelling and Tenderness Presentation
During palpation, use the second joint of the index finger to apply moderate pressure to the suspected area. If there is a noticeable withdrawal response or pain upon pressure, combined with a rise in local skin temperature, this often serves as direct evidence of periosteal inflammatory response. There is a simple testing method: before bed, mark the swollen area with a pen, and compare the spread in the morning.
Bruise Appearance Pattern
Subcutaneous bleeding caused by bone injury has a delayed characteristic. An outdoor enthusiast shared: 'After three days of high-altitude hiking, only then did the arch of my foot show purple bruises.' This phenomenon occurs because deep tissue bleeding takes time to permeate to the epidermis. If bruising presents a yellow-green hue, it indicates the injury has exceeded 72 hours.
Gait Compensation Mechanism
The human body instinctively adjusts walking posture to alleviate pressure on the affected area. By observing walking cycles in slow motion on a smartphone, note whether there is a shortening of the support phase on the affected side. A typical case: a basketball player developed a unique tiptoe running posture to reduce the load on the second metatarsal, ultimately leading to excessive strain on the Achilles tendon.
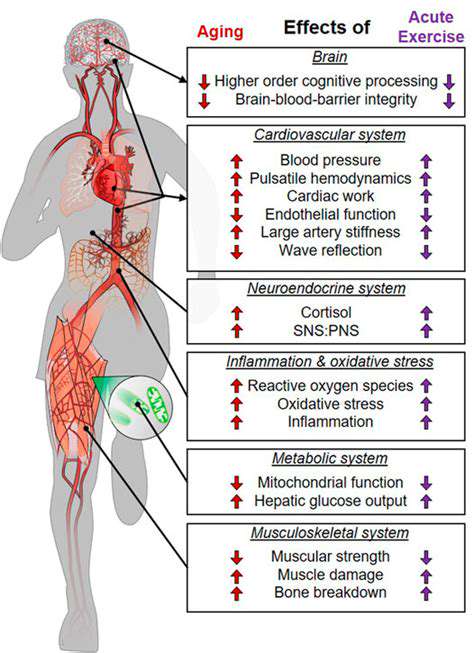
Fatigue Accumulation Effects
Microscopic bone injuries can affect energy transmission efficiency in the movement chain. Research shows that patients with stress fractures experience an average heart rate increase of 8-12 beats/minute during identical training, this increase in metabolic cost can serve as an early warning indicator. It is suggested to wear a sports watch to monitor changes in daily expenditure.
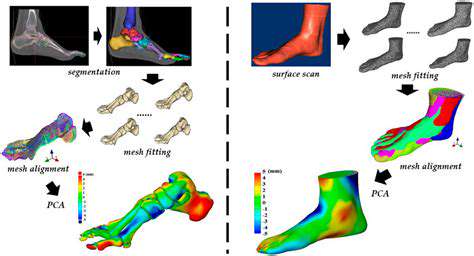
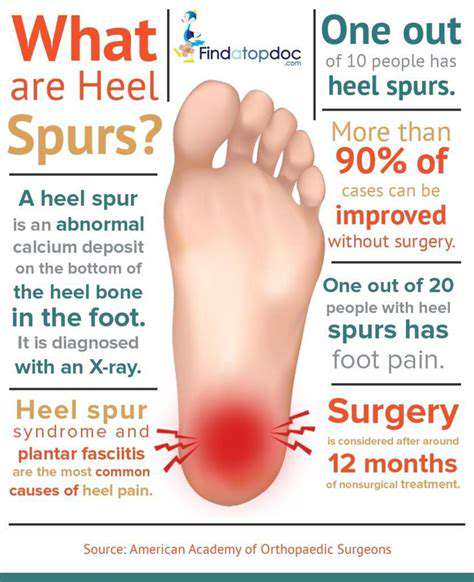
Imaging Diagnosis Progress
Although X-rays have a sensitivity of only 62% for early cracks, combined with 3D bone scanning, the detection rate can be increased to 89%. The latest ultrasound elastography technology can detect changes in bone density greater than 5%, which is particularly crucial for early intervention in athletes. Some team doctors reveal that they use weekly bone conduction testing to prevent seasonal injuries.
Understanding the Pain Patterns
Pain Evolution Trajectory
The typical development pattern is: onset of aching and soreness 2 hours after exercise → alleviation after 24 hours → reactivation during subsequent exercise. It is essential to record the advance of this 'pain clock'; when discomfort appears during the warm-up phase, it indicates that the injury has progressed to the second stage.
Characteristic Physical Signs
Single-leg jump tests are an effective self-assessment method: jump on the affected leg three times consecutively, and if it induces severe pain, the positive rate can be as high as 78%. Be sure to compare the intensity of pulse at the dorsalis pedis artery between both sides, as differences in blood circulation may suggest a stress fracture accompanied by compartment syndrome.
Environmental Influencing Factors
The combination of hard surfaces and cushioned running shoes creates a resonant effect. After changing the track material, a certain athletics team saw a 43% decrease in the incidence of stress fractures. It is recommended to alternate between training surfaces of varying hardness, similar to how cross-training balances muscle loads.
When to Seek Medical Attention
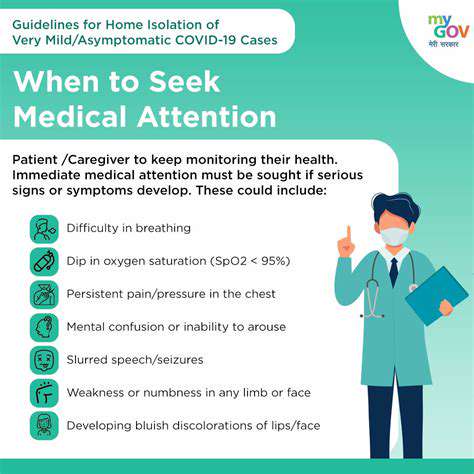
Emergency Indications
- Resting pain persists for more than 72 hours
- Nocturnal pain affects sleep quality
- Regular analgesics are ineffective
A commonly overlooked phenomenon: if pain interrupts sleep for more than three nights, the rate of bone healing can decrease by 27%. This is due to the importance of growth hormones secreted during deep sleep stages in repairing micro-injuries.
Rehabilitation Time Window
The first 14 days post-injury is a golden intervention period. Utilizing pulsed electromagnetic field therapy combined with vitamin K2 supplementation can shorten recovery time by 40%. Data from a rehabilitation center shows that when paired with the use of pressure-monitoring insoles, recurrence rates dropped from 31% to 9%.
Risk Factors for Stress Fractures
Biomechanical Risks
The risk for flat-footed individuals with a foot arch index below 0.25 is increased threefold. Using plaster molds to create customized orthotics can redistribute plantar pressure. After a marathon club introduced foot scanners, their seasonal injury rate decreased by 68%.
Nutritional Intervention Key Points
When vitamin D levels are below 30ng/ml, it is advised to supplement daily with 5000IU. A controlled experiment showed that a group taking collagen peptides for 8 weeks had a 73% improvement in bone density microstructure. Supplementing calcium with acidic fruit juice in the evening can boost absorption rates by 40%.
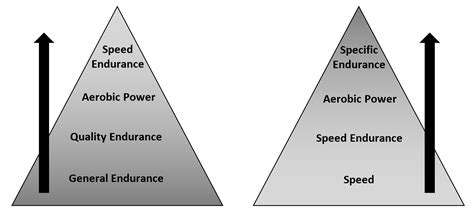
Training Load Formula
Using the acute-to-chronic workload ratio (ACWR) to monitor training intensity and keeping the ratio between 0.8-1.3 is the safest approach. A trail runner managed to maintain a record of no significant injuries over three years by controlling the increase in weekly running volume to no more than 10%.
Read more about Identifying Symptoms of Stress Fractures in the Foot
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options