Recognizing Early Signs of Rheumatoid Arthritis in the Feet
Differentiating RA Foot Pain from Other Conditions
Understanding the Common Symptoms
Spotting the early signs of rheumatoid arthritis (RA) foot pain is vital for timely treatment. Early diagnosis and intervention can dramatically alter the disease's trajectory, potentially preventing permanent joint destruction. Patients typically report aching and rigidity in foot joints, especially upon waking or after prolonged rest. This stiffness often lingers for half an hour or longer, disrupting routine activities.
In addition to stiffness and discomfort, many notice swelling and heat around affected joints. While these signs might seem minor at first, they intensify as RA progresses. Paying close attention to these initial warnings helps distinguish RA from other foot pain sources.
Differentiating RA from Other Types of Arthritis
While RA is one arthritis form, osteoarthritis represents another common type. The latter involves progressive cartilage deterioration, mainly impacting weight-bearing joints such as knees and hips. RA's hallmark is symmetrical joint involvement, affecting both sides simultaneously, whereas osteoarthritis often strikes joints unevenly.
Conditions like gout - caused by uric acid crystal accumulation - or infections can resemble RA symptoms. Medical professionals rely on blood analyses and imaging studies to identify specific inflammatory markers, enabling accurate differentiation between these conditions.
The Role of Medical Imaging in Diagnosis
X-rays serve as an initial diagnostic tool, revealing bone and joint abnormalities. However, they often fall short in assessing inflammation severity, a critical RA component. MRI scans excel at visualizing soft tissue inflammation, offering detailed joint structure images that aid RA confirmation.
Ultrasound technology provides real-time soft tissue imaging, capable of detecting early synovitis (joint lining inflammation) typical of RA. Combining these imaging methods with clinical evaluations creates a thorough diagnostic approach.
The Importance of Physical Examination
A rheumatologist's comprehensive physical assessment is indispensable for evaluating foot pain origins. The examination includes checking joints for swelling, sensitivity, and movement restrictions. Feeling for warmth and noting any structural abnormalities are equally important. These observations, paired with medical history, help guide subsequent diagnostic steps.
The Significance of Blood Tests in RA Diagnosis
Blood analysis proves essential in RA evaluation. Specific indicators like rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPA) often elevate in RA patients. While valuable for confirmation and monitoring, these markers might not appear during early disease stages.
Additional blood work, including complete blood counts and inflammatory markers (ESR and CRP), offers insights into systemic inflammation commonly accompanying RA. These tests complement other diagnostic methods, painting a complete clinical picture.
Lifestyle Modifications and Early Intervention
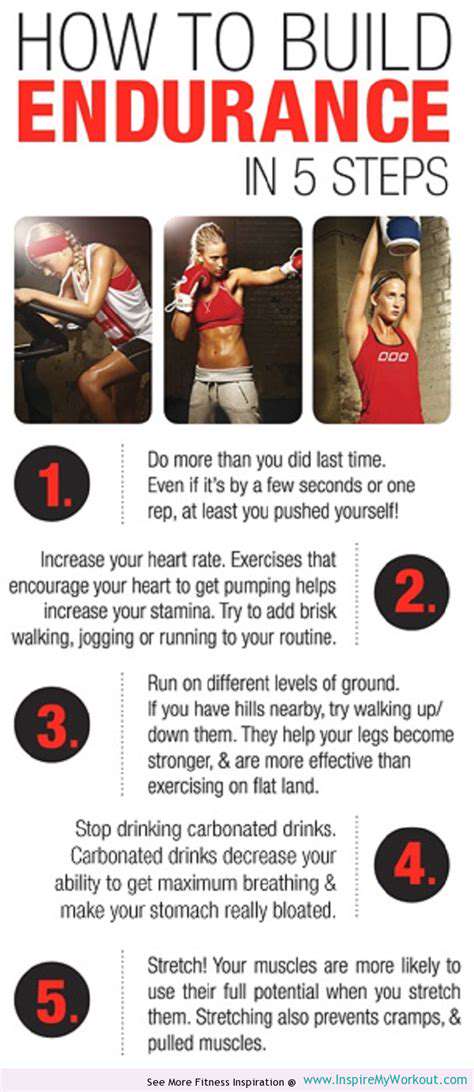
Prompt RA foot pain recognition and treatment are critical for preventing permanent joint damage and preserving mobility. Lifestyle adjustments - including joint-friendly exercise, anti-inflammatory nutrition, and sufficient rest - can significantly influence disease course. These modifications work synergistically with medical treatment to enhance symptom management and overall health.
Early DMARD (disease-modifying antirheumatic drug) initiation can stop disease advancement, reducing inflammation and protecting joint functionality. This proactive treatment strategy proves vital for minimizing RA's long-term effects and sustaining life quality.

Read more about Recognizing Early Signs of Rheumatoid Arthritis in the Feet
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health