Managing Arthritis in the Foot and Ankle
Diagnosing and Managing Your Arthritis
Getting the right diagnosis changed everything for me. My doctor didn't just glance at my swollen feet - she spent an hour examining every joint, asking about my family history, and ordering specific imaging tests. That MRI wasn't just pictures; it was a roadmap showing exactly where the damage was. Early detection isn't just about comfort - it's about preserving the joints you still have. I learned this the hard way after ignoring my symptoms for two years.
Management isn't about one magic solution - it's a toolkit. For me, that meant anti-inflammatory medications (with careful monitoring for stomach issues), water therapy (easier on the joints than regular exercise), and custom orthotics that felt strange at first but now I can't live without. The game-changer? Learning that losing just 10 pounds takes 40 pounds of pressure off my knees with every step. Small changes create big relief when you're consistent.
Here's what they don't tell you in brochures: your treatment plan will evolve. What worked last year might need adjusting now. I meet with my rheumatologist quarterly - not when I'm in crisis, but to stay ahead of problems. This proactive approach saved me from two potential surgeries already.

The Role of Medications in Arthritis Management
Pharmacological Approaches to Arthritis Management
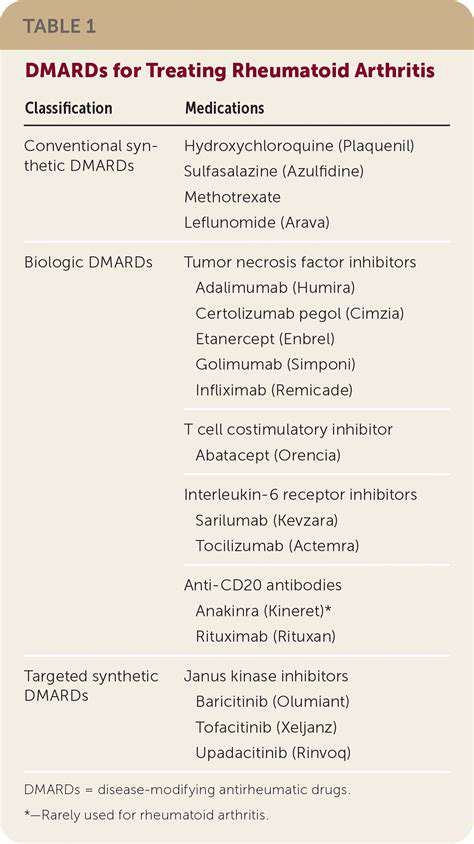
Medication strategies are as varied as arthritis symptoms themselves. In my decade of living with this condition, I've learned that NSAIDs are like fire extinguishers - great for immediate flare-ups but dangerous if overused. My gastroenterologist still scolds me about the ulcer I developed from taking ibuprofen like candy. The turning point came when my rheumatologist explained how DMARDs work - not just masking pain but actually slowing the disease's progression. It felt like going from putting out fires to preventing them.
Biologics were my last resort, and what a difference they made. The self-injections intimidated me at first, but the results - being able to walk my daughter to school again - made the weekly shots worthwhile. These medications aren't without risks (I caught every cold that first year), but for severe cases, they can be life-changing. Just last month, my lab results showed the first signs of remission in years.
Specific Medication Classes and Considerations
Corticosteroids taught me an important lesson: instant relief comes with long-term costs. After three months on prednisone, my face became moon-shaped and my bones became alarmingly fragile. Now we reserve them for extreme flares only. The medication dance is delicate - what helps your joints might harm your liver or kidneys. That's why my pharmacist reviews everything, even my herbal teas.
The most valuable advice I received? Keep a detailed medication journal. Tracking doses, side effects, and symptom changes helped my team fine-tune my regimen until we found the perfect balance. It's tedious work, but when you finally find that combination that lets you function normally again, every recorded detail feels worth it.
Footwear and Orthotic Support for Arthritis Relief
Choosing the Right Footwear
Finding proper shoes became my unexpected passion after wasting hundreds on pretty-but-painful options. The revelation? A thumb's width of space beyond your longest toe isn't a suggestion - it's a requirement. I learned the hard way that fashion sacrifices are temporary, but joint damage is permanent. My closet now holds exactly two pairs of dressy shoes - the rest are supportive sneakers in every color.
The material matters more than you'd think. Leather molds to your feet while providing support, unlike synthetic materials that can create painful pressure points. And that breaking in period? Myth. Shoes should feel comfortable immediately - if they don't, they never will.
Understanding Orthotic Support
Custom orthotics were my turning point. The process felt excessive at first - foam impressions, multiple fittings - but the results justified every step. These aren't just inserts; they're medical devices that redistribute pressure away from damaged joints. My podiatrist explained it like building a suspension system for my feet. Over-the-counter options can help too, but they're like reading glasses - fine for general use, but insufficient for specific needs.
Addressing Specific Arthritis Types
Rheumatoid arthritis taught me about mornings from hell - the hours it took for my swollen feet to fit into shoes. My solution? Velcro-adjustable shoes in multiple widths. For osteoarthritis sufferers, focus on shock absorption - I recommend shoes with gel or air cushioning. Your shoe needs change with your condition - reassess every six months.
Maintaining Foot Health and Hygiene
Simple habits prevent big problems. I keep a foot care kit with curved nail clippers (straight cuts invite ingrown nails), antifungal powder (damp feet breed infection), and a pumice stone (calluses alter gait). Neglecting foot care with arthritis is like ignoring oil changes in your car - eventually, everything breaks down.
Surgical Interventions in Advanced Cases

Minimally Invasive Procedures
When my doctor mentioned arthroscopy, I imagined science fiction. The reality? Three tiny incisions and home the same day. These procedures aren't miracles, but they can buy precious years of mobility. My sister-in-law's ankle scope gave her five extra years before needing a fusion - years she used to travel with her grandchildren.
Open Surgical Techniques
Joint replacement surgery terrified me until I met Martha at physical therapy. At 72, she'd had both knees and one hip replaced. The first month's hell, she admitted, but now I dance at my great-grandkids' weddings. Major surgery isn't failure - it's a strategic retreat to regain quality of life. The key is finding a surgeon who does hundreds of these procedures annually.
Post-Operative Care and Rehabilitation
Rehab is where battles are won or lost. I learned to celebrate small victories - first unassisted step, first full night's sleep. Physical therapy isn't optional - it's how you reclaim your life. My therapist modified exercises for my other arthritic joints, proving that smart rehab accommodates overall limitations.
Advanced Surgical Materials and Technologies
The new ceramic-on-polyethylene hip implants last decades longer than older models. Robotic-assisted surgery offers precision measured in millimeters. Today's surgical advances mean shorter recoveries and better long-term outcomes. Always ask your surgeon about the latest options - medicine evolves faster than textbook knowledge.