Diagnostic Techniques for Hand Disorders
Inspection
The first critical step when examining a patient's hand is a thorough visual inspection. This process requires keen attention to detail, as subtle changes in appearance can reveal significant underlying issues. During inspection, clinicians should carefully observe the hand's overall shape, looking for any visible abnormalities like unusual swelling, skin discoloration, or unusual markings. The skin's color and temperature provide particularly valuable information - cool, pale skin might suggest circulation problems, while warm, reddened areas could indicate inflammation.
Equally important is examining the alignment of bones and joints. Finger positioning and wrist structure often hold clues about past injuries or developing conditions. Observing how the hand moves during simple actions like making a fist or extending fingers helps assess joint function and identifies potential mobility restrictions.
Palpation
After visual inspection comes the hands-on examination. Palpation transforms observations into tangible findings through careful touch. Medical professionals systematically feel each part of the hand, checking bone structure, joint spaces, and soft tissues. This tactile examination reveals important details like unusual warmth, unexpected tenderness, or abnormal textures beneath the skin.
Checking pulses at the wrist provides direct information about blood flow to the hand. A weak or missing pulse warrants immediate attention as it may signal serious vascular issues. During palpation, examiners also search for unusual lumps or thickened areas, noting their exact location and characteristics.
Range of Motion (ROM) Assessment
Testing how the hand moves reveals much about its health. Each joint's full movement capacity tells a story about possible injuries or diseases. The examiner gently moves each finger and the wrist through their natural motions - bending, straightening, spreading, and rotating. Pain during movement or restricted motion often indicates specific problems needing further investigation.
Neurological Examination
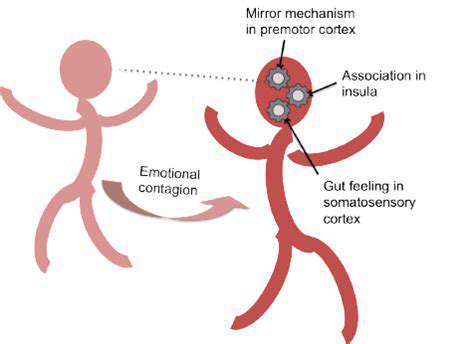
A complete nerve function check is essential. Testing sensation helps map potential nerve damage, with clinicians checking response to light touch, temperature, and vibration across different hand areas. Muscle strength tests evaluate nerve-muscle connections by having patients resist pressure during various hand movements.
Simple reflex tests provide additional neurological information. Abnormal reflexes often pinpoint specific nerve compression sites, guiding further diagnostic steps and treatment planning.
Special Tests
Targeted physical tests help confirm specific conditions. These specialized maneuvers reproduce symptoms to identify their source. For example, wrist flexion tests help diagnose carpal tunnel syndrome, while specific finger stability tests reveal ligament injuries. These focused examinations often provide the final pieces needed for an accurate diagnosis.
Vascular Examination
Assessing blood flow completes the hand examination. Checking pulse strength and capillary refill time reveals circulation quality. Observing skin color changes with position and watching for swelling helps identify potential vascular problems that might require specialized care.
Imaging Techniques: Visualizing the Inner Hand
Imaging Techniques: A Comprehensive Overview
Modern medical imaging provides windows into the body that physical examination alone cannot offer. These technologies continue advancing rapidly, giving doctors increasingly sophisticated ways to see inside the human body without surgery. Each imaging method serves specific purposes, from detecting broken bones to revealing subtle soft tissue abnormalities.
X-Ray Imaging: Early Pioneers of Visualization
The discovery of X-rays marked a revolution in medical diagnosis. This century-old technology remains indispensable for examining bone structure and detecting fractures. Modern digital X-ray systems produce clearer images with significantly less radiation than early machines, making the procedure safer while improving diagnostic accuracy.
Ultrasound Imaging: Sound Waves for Visual Displays
Using harmless sound waves, ultrasound creates moving images of internal structures. Its real-time capability makes it ideal for examining moving parts like heart valves or a developing fetus. Unlike X-rays, ultrasound poses no radiation risk, allowing repeated use when monitoring conditions over time.
Computed Tomography (CT) Scanning: Cross-Sectional Views
CT scanners combine multiple X-ray images to create detailed cross-sections. This technology excels at revealing internal injuries and abnormalities that standard X-rays might miss. The ability to reconstruct images in three dimensions helps surgeons plan complex procedures with greater precision.
Magnetic Resonance Imaging (MRI): Detailed Internal Views
MRI technology uses powerful magnets to produce exceptionally detailed images. For soft tissue evaluation, MRI often provides superior information compared to other imaging methods. Its ability to visualize nerves, ligaments, and brain tissue without radiation makes it invaluable for diagnosing many neurological and musculoskeletal conditions.
Nuclear Medicine Imaging: Radioactive Tracers
This specialized imaging tracks metabolic activity rather than just structure. By following radioactive tracers, doctors can identify areas of abnormal cell activity that might indicate cancer or other diseases. These scans provide functional information that complements the anatomical details from other imaging methods.
Interventional Imaging: Guiding Procedures
Real-time imaging transforms many medical procedures. Combining imaging with treatment allows precise, minimally invasive interventions. From placing stents to removing blood clots, these image-guided techniques reduce risks and recovery times compared to traditional surgery.
Read more about Diagnostic Techniques for Hand Disorders
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health