Hand Hygiene in Healthcare Professions
Specialized scenarios demand tailored approaches - surgical teams employ prolonged scrub protocols, while isolation units may require particular antiseptic solutions. Glove usage complements but never replaces proper hand cleansing, as improper removal frequently contaminates hands. Emerging technologies like persistent antimicrobial coatings and UV verification systems promise to revolutionize traditional practices.
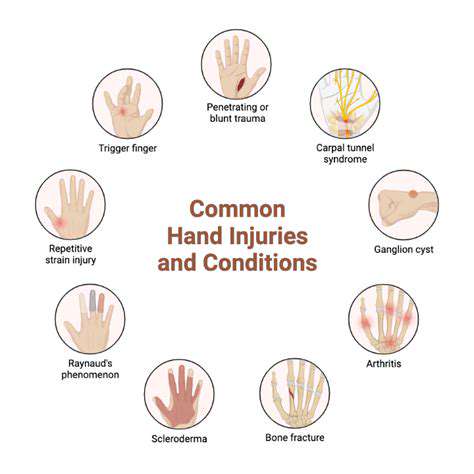
Pediatric and geriatric populations present unique challenges requiring creative solutions. From child-friendly educational tools to assisted washing stations for arthritic patients, inclusive design ensures everyone can participate in this fundamental health practice. These considerations become particularly crucial during outbreaks when entire communities must mobilize hygiene defenses.
Essential Hand Hygiene Techniques for Healthcare Professionals
Proper Handwashing Technique
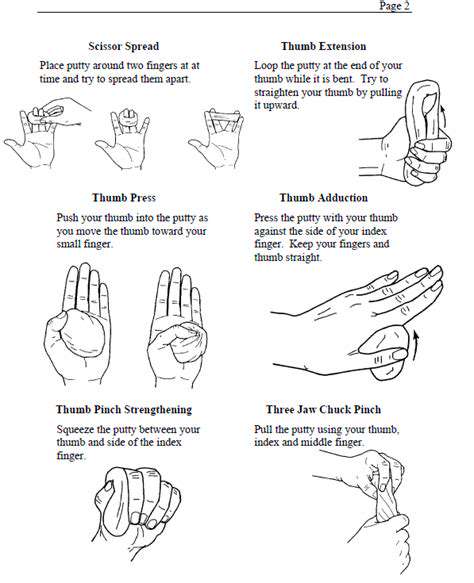
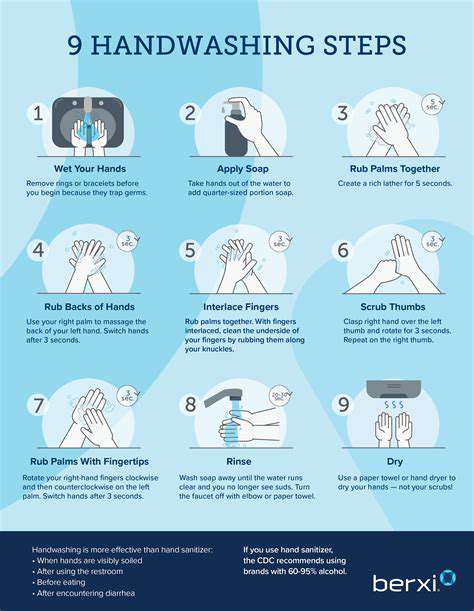
Clinical handwashing resembles a carefully choreographed dance, where each movement serves a specific cleansing purpose. The process begins with water temperature selection - warm enough to enhance soap efficacy but not so hot as to damage protective skin oils. Soap application should generate enough lather to cover all surfaces, with particular attention to thumbs and fingertips that most frequently contact contaminated surfaces.
Nail care proves surprisingly pivotal - subungual spaces harbor dense microbial populations requiring deliberate cleaning. Many facilities provide disposable nail cleaners at handwashing stations, while others mandate short, clean nails as employment requirements. Either approach recognizes this often-overlooked transmission vector.
Handwashing with Soap and Water
Traditional handwashing remains unsurpassed for removing both pathogens and organic material. The mechanical action of thorough rinsing proves particularly crucial for eliminating chlorine-resistant parasites like Cryptosporidium that alcohol can't address. Quality matters as much as technique - antimicrobial soaps with persistent activity offer advantages in high-risk settings, though proper use of any soap far outweighs minor formulation differences.
Drying method completes the process - disposable towels not only remove residual moisture where microbes thrive but also provide additional friction for pathogen removal. Air dryers, while environmentally friendly, may aerosolize contaminants if used improperly.
Hand Sanitizer Use
Modern alcohol-based rubs have transformed infection control when used appropriately. The key lies in applying sufficient volume (typically 3-5ml) to keep hands wet for the entire 20-30 second drying time. Burning sensations sometimes reported actually indicate proper application rather than cause for concern. Facilities should provide multiple sanitizer formulations to accommodate staff with skin sensitivities.
Hand Hygiene in Healthcare Settings
Hospital workflows must build hand hygiene moments into natural care sequences. Electronic medical record systems increasingly incorporate hand hygiene documentation alongside other vital signs, reinforcing its clinical importance. Some units employ colored hand stamps that fade with proper washing, providing visual feedback about technique effectiveness.
Leadership modeling proves critical - when senior clinicians visibly prioritize hand hygiene, compliance cascades through entire teams. Conversely, perceived double standards rapidly erode protocol adherence at all levels.
Alcohol-Based Hand Sanitizers
Formulation science continues advancing hand sanitizer technology. Newer emollient-enriched products combat the dryness and irritation that historically discouraged frequent use among healthcare workers. Some institutions now provide personalized sanitizer holsters, ensuring availability matches need while reducing cross-contamination risks at shared dispensers.
Importance of Hand Hygiene in Public Areas
Pandemic experiences permanently elevated public awareness about hand hygiene's community role. Transportation hubs now incorporate hygiene stations as standard infrastructure, much like waste receptacles or seating areas. Retailers recognizing customer expectations increasingly provide sanitizer at entrances and high-contact points, blending health protection with customer service.
School-based programs yield particularly high returns, instilling lifelong habits while reducing absenteeism. Creative approaches like glow germ demonstrations that make contamination visible under UV light powerfully reinforce abstract concepts for young learners.
The Impact of Hand Hygiene on Reducing Healthcare-Associated Infections and Improving Patient Outcomes
Hand Hygiene: A Cornerstone of Infection Control
Microscopic battles rage on caregivers' hands, where proper technique means the difference between healing and harm. Evidence demonstrates that consistent hand hygiene adherence could prevent up to half of all healthcare-associated infections. This startling statistic underscores why leading hospitals treat hand cleanliness with the same seriousness as medication administration protocols.
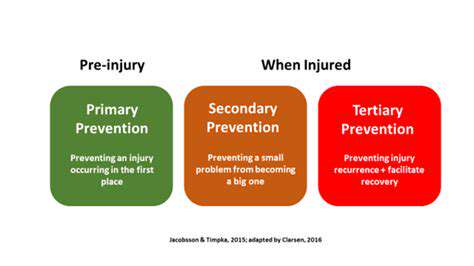
Standardization drives success - the clearest reduction in HAIs occurs when facilities implement the WHO's Five Moments framework systemwide. This approach moves beyond vague encouragement to specific, situation-based guidance that staff can consistently apply across diverse clinical scenarios.
The Link Between HAIs and Poor Hand Hygiene
Pathogens exploit lapses in hand hygiene with frightening efficiency. A single skipped handwash can initiate transmission chains affecting dozens of vulnerable patients. The most troubling infections often trace back to these preventable breaches, with multidrug-resistant organisms posing particular concerns.
Human factors complicate compliance - fatigue, cognitive overload, and competing priorities all contribute to unintentional lapses. Smart system design anticipates these challenges through ergonomic station placement, intuitive reminders, and streamlined product access that makes proper hygiene the path of least resistance.
Improving Patient Outcomes Through Hand Hygiene
The clinical benefits of rigorous hand hygiene programs extend far beyond infection metrics. Surgical patients in facilities with strong compliance experience better wound healing and fewer readmissions. Neonatal units see improved weight gain and development when hand protocols are strictly enforced. Even antibiotic stewardship improves as prevention reduces unnecessary prescriptions.
Financial analyses consistently show hand hygiene programs deliver exceptional ROI - every dollar invested in improved compliance yields multiple dollars in averted treatment costs. These savings compound as reduced infection rates decrease length of stay, freeing capacity for additional patients.
Strategies for Enhancing Hand Hygiene Adherence
Behavioral science informs the most effective compliance strategies. Peer accountability programs often outperform top-down mandates, especially when paired with transparent unit-level reporting. Some institutions implement hand hygiene champions - respected clinicians who model ideal practices while gently correcting colleagues.
Technology increasingly supports these efforts - wearable reminders, real-time monitoring systems, and even smartphone apps help maintain focus on this repetitive but critical task. The most sophisticated systems integrate with electronic health records to correlate hand hygiene events with patient outcomes.
The Role of Education and Training
Effective education moves beyond rote demonstrations to address the why behind the how. When clinicians understand exactly how their actions prevent specific infections in identifiable patients, compliance transforms from obligation to professional pride. Simulation training that visually demonstrates contamination spread proves particularly impactful.
Monitoring and Evaluation for Continuous Improvement
Data-driven approaches yield the most sustainable results. Leading institutions track not just overall compliance rates but specific opportunity types, identifying patterns that reveal systemic barriers. Unit-specific dashboards allow targeted interventions where needed most, while celebrating areas of excellence.
The most progressive facilities incorporate patient feedback into their monitoring - after all, no one has greater motivation to ensure proper hand hygiene than those whose lives depend on it. This patient partnership model fosters mutual accountability and continuous culture improvement.