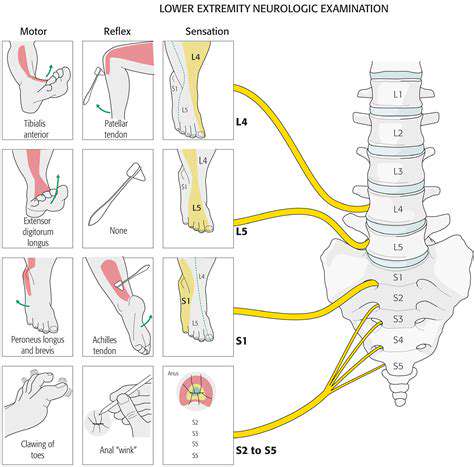
Addressing Nerve Pain in the Lower Extremities
The Role of Medications in Nerve Pain Relief
Medications for Nerve Pain Management
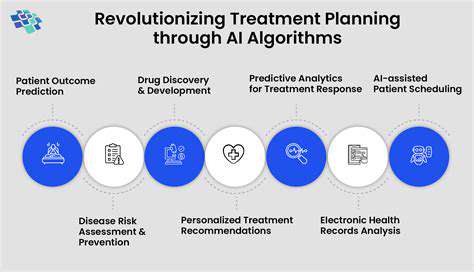
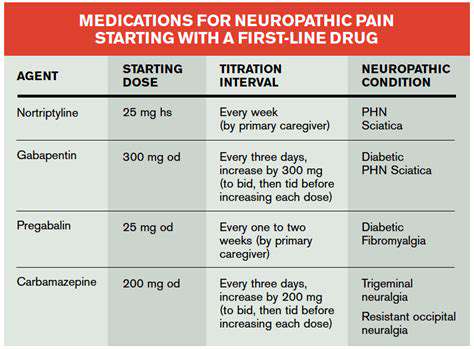
Medications are indispensable tools when it comes to tackling the complex challenge of neuropathic pain. Unlike typical pain, this condition stems from misfiring nerves that send distorted signals to the brain. The key to successful treatment lies in personalized care plans that address each patient's unique pain profile. Modern pharmacology offers multiple pathways to relief, targeting everything from nerve inflammation to signal transmission. Many patients find optimal results through carefully balanced combination therapies, though this requires close medical supervision to manage potential side effects. Regular follow-ups allow doctors to fine-tune treatment as the condition evolves.
The pharmaceutical arsenal against nerve pain includes diverse options with distinct advantages. While opioids remain controversial due to dependency risks, they still serve an important role for refractory cases when other treatments fail. Many specialists prefer starting with neuromodulators like certain antidepressants that can recalibrate pain perception at the nervous system level. The journey to effective pain control often involves methodical experimentation under professional guidance, as individual biochemistry significantly influences drug response.
Types of Medications and Their Mechanisms
Medical science categorizes nerve pain medications by their biochemical interactions. Some antidepressants, particularly older tricyclics and newer SNRIs, demonstrate remarkable efficacy by adjusting neurotransmitter levels that govern pain interpretation. These drugs can essentially turn down the volume on persistent pain signals, offering many patients substantial improvement in quality of life.
Anticonvulsant medications bring a different approach, stabilizing erratic nerve activity that contributes to neuropathic discomfort. For conditions like diabetic neuropathy or postherpetic neuralgia, these drugs often become first-line treatments due to their targeted mechanism. The selection process weighs multiple clinical factors including pain characteristics, medical history, and each drug's safety profile.
Topical treatments present a localized alternative that minimizes whole-body exposure. Formulations containing numbing agents or anti-inflammatory compounds can provide focused relief for surface-level nerve pain. While convenient, their effectiveness depends heavily on pain location and depth, making them more suitable for certain conditions than others.
This educational overview cannot replace professional medical consultation. Always seek qualified healthcare advice for proper diagnosis and treatment of nerve-related pain conditions.
Lifestyle Adjustments for Long-Term Pain Management

Prioritizing Sleep
Sleep quality directly correlates with pain perception and recovery. Maintaining consistent sleep-wake times trains the body's internal clock, while pre-bed relaxation rituals prepare the nervous system for rest. Quality sleep acts as natural medicine, reducing inflammation and improving pain tolerance. Strategic avoidance of stimulants and alcohol near bedtime preserves sleep architecture, while proper sleep environment setup addresses physical comfort needs.
Individual sleep requirements vary, but investing in supportive bedding and optimizing bedroom conditions (cool, dark, quiet) benefits nearly everyone. Those with chronic pain may need additional sleep hygiene adjustments to overcome discomfort-related sleep disruptions.
Nourishing Your Body
Nutritional choices create the biochemical foundation for nerve health and pain modulation. Whole foods provide the building blocks for nerve repair, while processed items often promote inflammation. A nutrient-dense, anti-inflammatory diet serves as powerful adjunct therapy for chronic pain conditions. Regular meal timing stabilizes energy metabolism, preventing the blood sugar swings that can exacerbate pain sensitivity.
Hydration maintains optimal nerve function by facilitating nutrient transport and waste removal at the cellular level. Many patients find that simply increasing water intake improves their baseline pain levels.
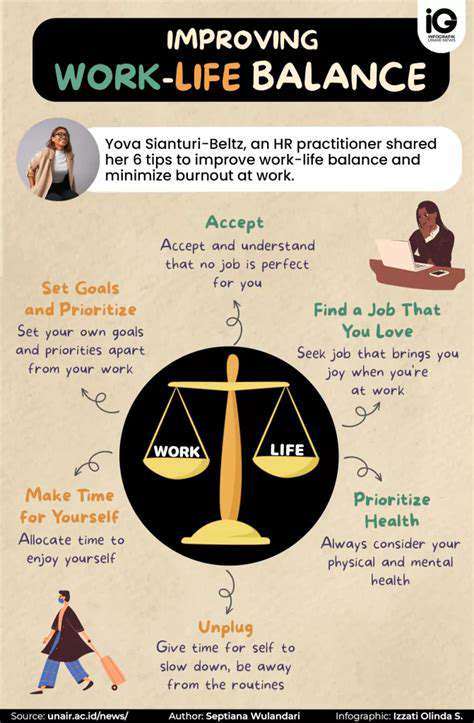
Managing Stress
The stress-pain connection forms a vicious cycle that requires active management. Mindfulness practices rewire the brain's pain processing centers, while enjoyable hobbies provide natural dopamine boosts that counteract discomfort. Effective stress reduction breaks the biochemical chain reactions that amplify pain signals. Professional counseling can provide additional tools for those dealing with trauma or anxiety-related pain components.
Regular Physical Activity
Movement therapy remains one of the most underutilized pain management tools. Appropriate exercise stimulates natural painkillers (endorphins) while improving circulation to damaged nerves. Consistent physical activity rebuilds functional capacity while reducing central nervous system hypersensitivity. The key lies in finding sustainable activities that accommodate current limitations while progressively rebuilding strength and mobility.
Cultivating Healthy Relationships
Social support buffers against the psychological toll of chronic pain. Meaningful connections release oxytocin, a hormone that naturally dampens pain signals. Strong social networks correlate with better pain coping skills and treatment adherence. Open communication about pain-related needs helps loved ones provide appropriate support without enabling disability.
Prioritizing Mental Wellness
The mind-body connection in pain management cannot be overstated. Cognitive-behavioral techniques help reframe pain perception, while nature exposure reduces stress hormones. Mental health maintenance is not secondary to physical treatment - it's an integral component of comprehensive pain care. Professional mental health support should be sought as readily as medical treatment for physical symptoms.
Creating a Supportive Environment
Environmental design significantly impacts pain experience. Ergonomic adjustments reduce physical strain, while positive social atmospheres improve pain tolerance. Intentional environment shaping removes unnecessary stressors that exacerbate pain perception. This includes both physical spaces and social circles, with careful boundary setting to preserve energy for healing.
Read more about Addressing Nerve Pain in the Lower Extremities
Hot Recommendations
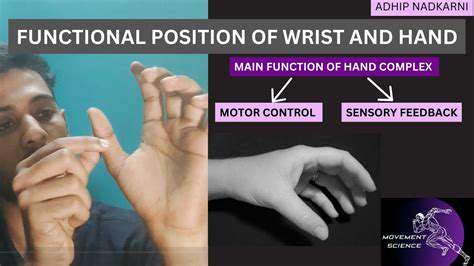
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health