The Role of Vitamin D in Bone Strength
Vitamin D directly communicates with bone-building osteoblasts through specialized receptors. This conversation triggers production of bone matrix proteins, resulting in denser, more resilient bone architecture. The vitamin's presence determines whether osteoblasts work at full capacity or operate below potential.
The vitamin's influence spans the entire bone formation process - from regulating growth patterns to ensuring proper mineralization of new bone tissue. Such comprehensive involvement explains why vitamin D deficiency shows such dramatic effects on skeletal development.
Bone Remodeling: Osteoclasts and Vitamin D's Role
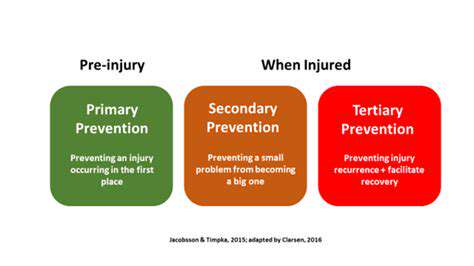
Our skeletons constantly rebuild themselves through remodeling cycles. While osteoclasts break down aged bone, vitamin D serves as the project manager, keeping demolition crews in check. This regulatory function prevents excessive bone loss while allowing necessary structural updates throughout our lives.
Vitamin D Deficiency and Bone Health Risks
Inadequate vitamin D creates perfect conditions for bone disorders to develop. Adults face higher osteoporosis risk - bones become porous like Swiss cheese, fracturing unexpectedly. Elderly individuals prove especially vulnerable as aging naturally reduces vitamin D production efficiency.
Children's developing skeletons suffer differently, with deficiency potentially causing rickets. This condition softens bones, sometimes leading to visible deformities that underscore vitamin D's critical role in pediatric bone development.
Vitamin D and Overall Bone Health
The vitamin's bone benefits extend beyond basic formation and maintenance. Optimal levels create fracture-resistant bones that better withstand life's physical demands. This protective effect grows increasingly valuable as we age, helping preserve mobility and independence when bones naturally weaken.
Maintaining proper vitamin D status represents one of the most effective strategies against age-related bone loss. The difference shows in reduced fracture rates and maintained quality of life across decades. No other nutrient impacts skeletal resilience so profoundly.
Sources of Vitamin D and Dietary Recommendations
Sources of Vitamin D from Sunlight
Sunlight remains nature's vitamin D factory, with skin synthesizing the nutrient upon UVB exposure. Production rates vary dramatically based on geography, season, time of day, and individual skin characteristics. Darker complexions naturally filter more UV radiation, requiring longer exposure for equivalent vitamin D synthesis compared to fair-skinned individuals.
While sunshine offers free vitamin D, smart exposure matters. Brief midday sessions (10-30 minutes for most adults) often suffice without risking skin damage. Cloudy climates or winter months typically necessitate alternative sources to maintain adequate levels.
Dietary Sources of Vitamin D
Few foods naturally contain significant vitamin D amounts. Fatty fish like wild salmon and mackerel top the list, with a single serving providing several days' requirements. Pasture-raised egg yolks deliver smaller but meaningful amounts, while mushrooms exposed to UV light can provide plant-based vitamin D.
Food fortification bridges the gap for many. Nearly all U.S. milk gets fortified, as do many cereals, orange juices, and plant milks. Regular consumption of these enhanced foods helps maintain baseline vitamin D status between sun exposure opportunities.
Vitamin D Supplements
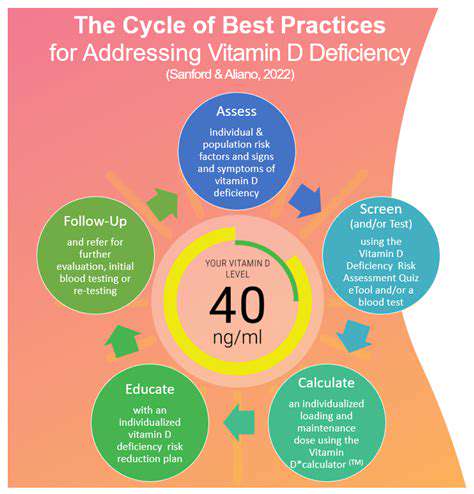
When sunlight and diet fall short, supplements offer reliable insurance. Available as D2 (plant-derived) or D3 (animal-derived), these come in various potencies. Medical guidance proves essential - excessive supplementation carries risks while too little fails to correct deficiencies. Blood testing helps personalize dosing for optimal results.
Factors Affecting Vitamin D Absorption
Absorption efficiency depends on multiple variables. Digestive disorders like celiac disease impair fat-soluble vitamin uptake, while obesity sequesters vitamin D in fat tissue. Certain medications including steroids and weight-loss drugs can interfere with metabolism. Even sunscreen use, while critical for skin cancer prevention, reduces cutaneous vitamin D production.
Dietary Recommendations for Vitamin D
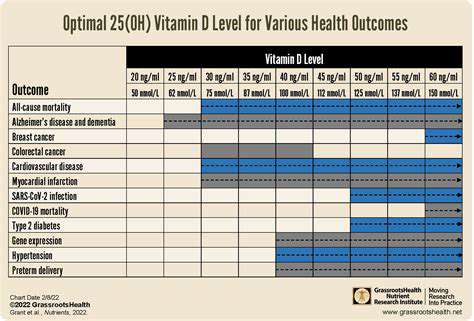
Current guidelines suggest 600-800 IU daily for most adults, with higher amounts (800-1000 IU) recommended for seniors. However, individual needs vary based on baseline status, sun exposure, and health conditions. Periodic blood tests (measuring 25-hydroxyvitamin D) provide the only accurate assessment of vitamin D adequacy.
Importance of Vitamin D in Bone Health
Vitamin D functions as the gatekeeper for calcium utilization, determining how much dietary calcium actually benefits bones. Without it, calcium passes through the body unused, regardless of intake quantity. This explains why calcium supplements alone often fail to improve bone density without concurrent vitamin D sufficiency.
Interactions with Other Nutrients
Vitamin D works best with nutritional teammates. Magnesium activates the vitamin's metabolic pathways, while vitamin K directs calcium to bones rather than arteries. Adequate protein intake provides structural material for bone matrix formation. This nutrient synergy explains why whole-food approaches often outperform isolated supplementation for bone health.