Managing Peripheral Artery Disease in the Legs
What is Peripheral Artery Disease (PAD)?
Understanding the Basics
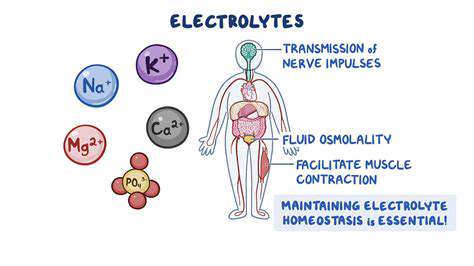
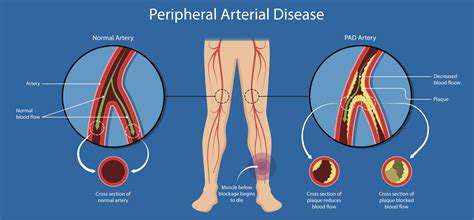
Peripheral artery disease (PAD) is a widespread circulatory issue impacting blood vessels beyond the heart and brain. When arteries supplying blood to limbs like legs and feet narrow or clog, blood flow diminishes, triggering symptoms and complications. Grasping PAD's root causes proves vital for proper care. Detecting it early and treating it promptly helps avoid severe outcomes.
Atherosclerosis, the accumulation of plaque in arteries, frequently underlies PAD. This plaque consists of cholesterol, fats, and other materials. Gradually, it hardens and constricts arteries, impeding blood flow. Habits like smoking, hypertension, and elevated cholesterol dramatically raise PAD risks.
Symptoms and Diagnosis
PAD symptoms vary widely; some people notice none at all. Initial signs often involve leg or buttock cramps, pain, or tiredness during activity, easing with rest. Many mistakenly attribute these early warnings to aging or poor fitness.
Doctors typically begin with a physical exam, checking pulses, skin tone, and temperature. Advanced tests like ankle-brachial index (ABI) or angiography may follow to confirm PAD and gauge its severity.
Risk Factors and Prevention
Smoking, hypertension, high cholesterol, diabetes, and family history elevate PAD risks. Staying active, eating well, and maintaining a healthy weight are key to prevention.
For diabetics, tight blood sugar control is especially critical to curb PAD progression. Quitting smoking offers one of the strongest protective effects. Routine doctor visits enable early PAD detection and intervention.
Treatment Options
PAD treatment aims to ease symptoms, slow disease advancement, and prevent complications. Lifestyle adjustments like exercise and diet changes form the foundation.
Doctors may prescribe blood pressure drugs or statins to improve circulation. Severe cases might require angioplasty or bypass surgery. Treatment plans are tailored to each patient's unique situation.
Impact on Daily Life
PAD can disrupt daily routines, causing pain, exhaustion, and limited mobility. Tasks like walking or climbing stairs may become challenging. Improving blood flow and managing symptoms helps people stay active and engaged in life.
Complications and Prognosis
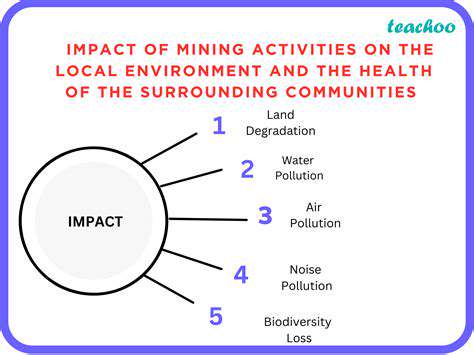
Without treatment, PAD may lead to amputations, heart attacks, or strokes. Outcomes depend on disease severity, treatment success, and coexisting conditions. Catching PAD early and treating it aggressively greatly improves prognosis.
Consistent monitoring and treatment adherence are crucial. The ultimate goal is symptom relief, complication prevention, and preserved quality of life.
Living with PAD
Managing PAD demands active participation through diet, exercise, and medication compliance. Sticking to prescribed treatments and attending regular checkups makes a real difference.
Support networks and educational materials offer practical help. Sharing experiences with fellow PAD patients provides both emotional support and useful tips.
Lifestyle Modifications for PAD Management
Dietary Changes
Heart-healthy eating plays a central role in PAD care. Emphasize fruits, vegetables, whole grains, and lean proteins while cutting back on saturated fats, cholesterol, and salt. This approach supports cardiovascular health and slows PAD progression.
Antioxidant-rich foods like berries and fiber-packed greens benefit blood vessels. Minimizing processed foods and sugary beverages matters equally. Nutritionists can create customized meal plans for lasting results.
Exercise Regimen
Regular movement boosts circulation and alleviates PAD symptoms. Target 30 minutes of moderate activity most days—walking, cycling, or swimming work well. Always consult your physician before beginning new exercises, particularly with advanced PAD.
Start slow and build up gradually. Even brief activity sessions help. Pay attention to your body's signals and modify intensity as needed.
Smoking Cessation
Tobacco use severely aggravates PAD by harming blood vessels and limiting blood flow. Kicking the habit ranks among the most impactful steps for PAD patients. Nicotine constricts vessels and reduces limb oxygenation, worsening symptoms.
Quitting benefits extend well beyond PAD, enhancing heart health and lung function. Healthcare providers can suggest effective cessation strategies.
Stress Management Techniques
Chronic stress promotes inflammation and vessel constriction, potentially intensifying PAD. Relaxation practices like meditation, deep breathing, or yoga help counteract these effects.
Such activities lower blood pressure and stress hormones. Discovering enjoyable stress-relievers forms an important part of comprehensive PAD care.
Blood Pressure Control
Keeping blood pressure in check protects blood vessels from further damage. This often requires medication alongside dietary changes, exercise, and stress reduction.
Blood Sugar Control (For Diabetics)
Diabetics must vigilantly manage glucose levels to protect against PAD complications. Consistent blood sugar monitoring, diabetes-friendly eating, and medication adherence are non-negotiable. Regular endocrinologist visits ensure proper management.
Read more about Managing Peripheral Artery Disease in the Legs
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health