Preventing Falls Through Foot Care in the Elderly
Assessing Foot Health in Seniors: Common Issues
Foot health maintenance assumes critical importance for older adults, as podiatric issues can dramatically influence mobility and independence. Aging brings physiological changes like diminished circulation, muscular atrophy, and structural foot alterations that predispose seniors to various podiatric concerns. These age-related transformations increase vulnerability to infections, ulcerations, and traumatic injuries. Early recognition and intervention become paramount for preventing debilitating complications and preserving autonomy.
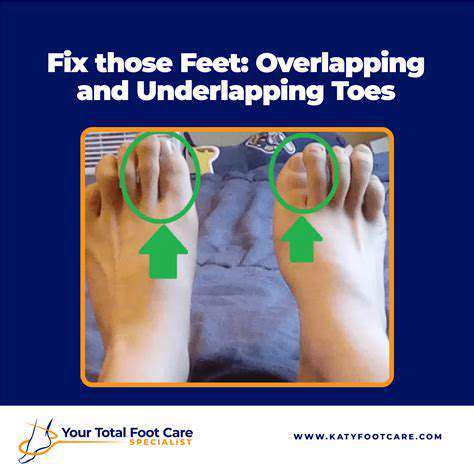
Frequently encountered conditions include bunions, hammertoes, and the aforementioned plantar fasciitis, each capable of causing significant discomfort and functional limitations. Thoughtful footwear selection provides foundational support for aging feet, alleviating pressure points and enhancing stability. Routine podiatric assessments facilitate early problem identification and customized treatment strategies, forming the cornerstone of preventive foot care for older populations.
Systemic health conditions further complicate senior foot health. Diabetes mellitus, through its neuropathic and vasculopathic effects, elevates risks for foot ulcers and infections. Arthritic conditions impair joint mobility while contributing to chronic pain. Recognizing these systemic influences proves essential for delivering comprehensive, effective foot care. The interplay between general health and foot wellness demands consideration in any thorough geriatric assessment.
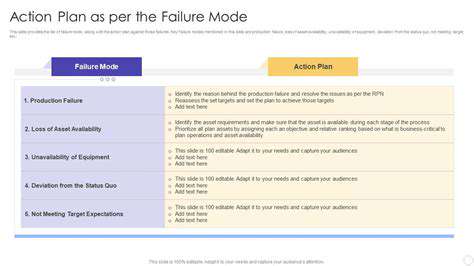
Risk Factors and Prevention Strategies
Multiple factors converge to increase seniors' podiatric vulnerability. Diminished protective sensation, whether from aging or conditions like diabetes, allows minor injuries to progress unnoticed. Compromised circulation, another common age-related change, delays healing and increases infection risks. Medication side effects may also impact foot health, underscoring the importance of thorough medication reviews with healthcare providers.
Preventive measures form the first line of defense in senior foot care. Daily foot inspections should become routine, with attention to skin integrity, temperature changes, and nail condition. Footwear selection requires careful consideration of support, fit, and non-slip properties. Weight optimization reduces mechanical stress on foot structures. Nutritional adequacy supports tissue health and wound healing capacity.
Regular physical activity, even gentle walking, enhances circulation and maintains foot strength. For diabetic individuals, meticulous glucose control significantly reduces complication risks. Professional podiatric guidance ensures appropriate, individualized preventive strategies. These combined efforts can dramatically improve foot health outcomes and quality of life for older adults.
Maintaining Healthy Feet: Essential Practices for Fall Prevention
Footwear Selection: A Crucial Factor
Appropriate footwear selection represents one of the most modifiable fall risk factors for older adults. Ideal shoes combine proper fit, non-slip soles, and adequate support while avoiding excessive heel height or instability. Regular shoe inspections identify wear patterns indicating replacement needs, particularly regarding sole traction and structural integrity.
Activity-specific footwear choices matter greatly. Walking shoes differ from athletic trainers in their support patterns, and both differ from dress shoes. The common denominator should be stability, comfort, and non-slip properties. Trying shoes later in the day, when feet tend to swell slightly, helps ensure proper fit throughout daily wear.
Regular Foot Examinations: Early Detection is Key
Routine podiatric evaluations serve as preventive maintenance for aging feet. These assessments can identify developing problems like structural deformities or dermatologic issues before they significantly impact mobility. Early intervention often prevents minor issues from becoming major obstacles to stability and independence.
During examinations, gait analysis provides valuable insights into weight distribution and potential imbalance sources. Custom orthotics or specific exercises may be recommended to address identified issues. This proactive approach to foot health maintenance helps preserve mobility and reduce fall risks.
Maintaining Good Posture: Body Awareness for Balance
Postural awareness significantly influences balance and fall risk. Conscious attention to spinal alignment and weight distribution through the feet enhances stability during movement. Simple practices like chin tucks and shoulder blade squeezes can improve overall posture when performed regularly.
Core strengthening exercises complement postural improvements by providing better trunk control. This enhanced stability proves particularly valuable when navigating uneven surfaces or recovering from minor balance disturbances. Postural training should be incorporated gradually into daily routines for sustainable benefits.
Addressing Foot Pain: Prompt Treatment is Vital
Persistent foot discomfort warrants professional evaluation rather than dismissal as inevitable aging. Various treatment modalities exist for common podiatric conditions, ranging from physical therapy to minimally invasive procedures. Delaying evaluation often allows problems to progress, increasing treatment complexity and recovery time.
Pain management strategies should address both symptoms and underlying causes for optimal results. Temporary accommodations like activity modification or assistive devices may be recommended during treatment phases. The goal remains restoring pain-free function to maintain mobility and independence.
Proper Foot Care Habits: Daily Routines for Healthy Feet
Consistent foot hygiene practices form the foundation of preventive care. Thorough daily cleaning, careful drying (especially between toes), and appropriate moisturizing maintain skin integrity. Nail care requires particular attention, with straight-across trimming to prevent ingrown nails.
Regular self-examinations facilitate early problem detection. Using a mirror to visualize all foot surfaces helps identify changes that might otherwise go unnoticed. Any persistent abnormalities should prompt professional evaluation rather than self-treatment attempts.
Environmental Considerations: Safeguarding Your Surroundings
Home environment modifications significantly reduce fall risks. Key interventions include removing loose rugs, improving lighting (particularly along nighttime pathways), and installing grab bars in critical areas like bathrooms. Floor surfaces should be evaluated for slip resistance, with non-slip treatments applied where needed.
Outdoor navigation requires similar precautions. Attention to surface conditions, use of appropriate footwear for weather conditions, and consideration of mobility aids when warranted all contribute to safer community ambulation. Planning routes to avoid known hazards represents another simple yet effective strategy.
Houston's offensive execution demonstrates remarkable synergy, blending transition excellence with perimeter marksmanship. Jalen Green's ability to penetrate defenses and create opportunities under duress showcases elite-level skill, frequently delivering in high-leverage situations. The squad's unselfish ball movement, evidenced by their impressive assist numbers, consistently disrupts opposing defensive schemes.
Read more about Preventing Falls Through Foot Care in the Elderly
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health