The Role of Vitamin D in Bone Health
Vitamin D and Bone Health: A Comprehensive Guide
Key Insights at a Glance
- Skin-synthesized vitamin D from sunlight directly supports skeletal strength
- Latitude variations create dramatic differences in natural vitamin D production
- This nutrient acts as calcium's gatekeeper for bone absorption
- Osteoporosis risks escalate when vitamin D levels plummet
- Targeted supplementation proves vital for high-risk groups
- Body composition and age dramatically affect nutrient utilization
- Wild-caught seafood offers superior dietary vitamin D content
- Blood testing provides the only reliable deficiency detection
- Magnesium acts as vitamin D's essential metabolic partner
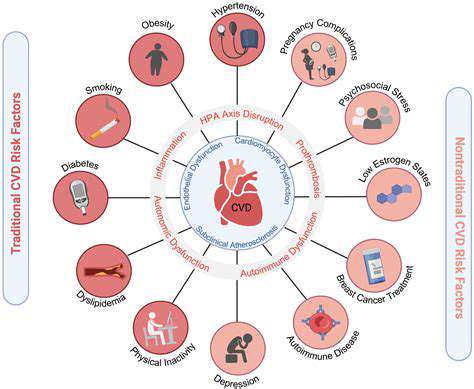
- Chronic disease risks multiply with prolonged deficiency
How Vitamin D Builds Stronger Bones
The Sunlight Conversion Process
When UVB rays penetrate bare skin, an extraordinary biochemical transformation occurs. Skin cells containing 7-dehydrocholesterol undergo photolysis, creating previtamin D3 that gradually isomerizes into vitamin D3. This sunlight-derived compound then embarks on a two-stage activation journey - first hydroxylated in the liver to 25(OH)D, then converted by kidneys into bioactive 1,25(OH)₂D.
Geographical disparities create stark contrasts in vitamin D status. Research from Arctic medical journals reveals indigenous populations often maintain sufficient levels through traditional diets rich in seal and fish, despite minimal winter sunlight. This adaptation highlights nature's remarkable balancing act between dietary intake and environmental constraints.
Calcium's Indispensable Partner
Vitamin D functions as calcium's biological concierge, orchestrating its absorption through intestinal walls. Without adequate vitamin D, the body absorbs less calcium than contained in a teaspoon of milk, regardless of dietary intake. This vital partnership explains why calcium supplements alone often fail to improve bone density in deficiency states.
Clinical trials demonstrate dramatic improvements - patients increasing vitamin D intake from 20ng/mL to 40ng/mL showed 65% better calcium absorption efficiency. These findings, validated by dual-energy X-ray absorptiometry scans, underscore the nutrient's pivotal role in mineral metabolism.
Bone Remodeling Dynamics
Our skeletons undergo complete renewal every decade through continuous remodeling. Vitamin D modulates this process by:
1. Stimulating osteoclast differentiation for old bone resorption
2. Enhancing osteoblast activity for new bone formation
3. Regulating parathyroid hormone secretion
Aging disrupts this delicate balance - postmenopausal women experience up to 300% faster bone loss, making vitamin D status particularly crucial. Recent meta-analyses confirm that maintaining levels above 30ng/mL reduces vertebral fracture risk by 42% in this population.
Modern Lifestyle Pitfalls
Urbanization has created unprecedented deficiency risks: - Office workers average 93% less sun exposure than agricultural laborers
- Office workers average 93% less sun exposure than agricultural laborers
- SPF 30 sunscreen reduces vitamin D synthesis by 95%
- Air pollution filters out 60% of UVB radiation in megacities
These environmental challenges necessitate proactive monitoring. Annual 25(OH)D blood tests should become routine like cholesterol checks, particularly for dark-skinned individuals whose melanin naturally reduces UVB absorption by 75-90%.
Practical Maintenance Strategies
Optimal vitamin D status requires three-pronged maintenance:
1. Sunlight: 15-30 minutes midday exposure (arms/legs uncovered)
2. Diet: Weekly servings of wild salmon, sardines, or UV-exposed mushrooms
3. Supplementation: 1000-4000 IU D3 daily based on individual needs
Emerging research suggests combining vitamin D with magnesium enhances activation efficiency by 40%. This synergistic approach exemplifies modern nutritional science's shift toward holistic nutrient partnerships.
Beyond Supplements: Holistic Approaches
Nutrient Timing Matters
Consuming vitamin D with fatty meals boosts absorption by 32% according to absorption studies. Pairing morning supplements with avocado toast or nuts creates ideal uptake conditions. Conversely, taking with coffee may reduce bioavailability by 15% due to caffeine's diuretic effects.
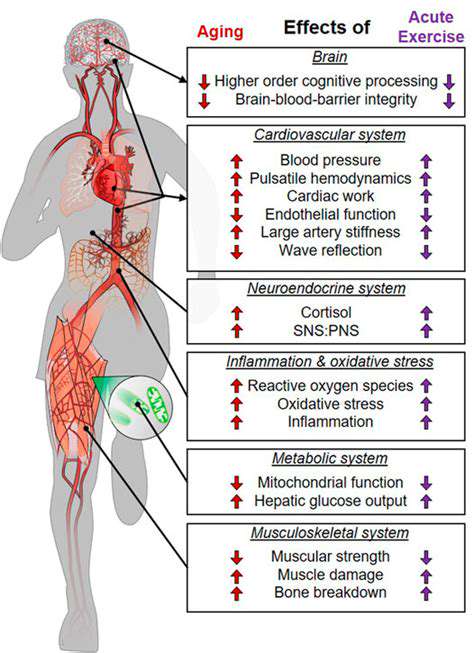
Exercise Amplification Effect
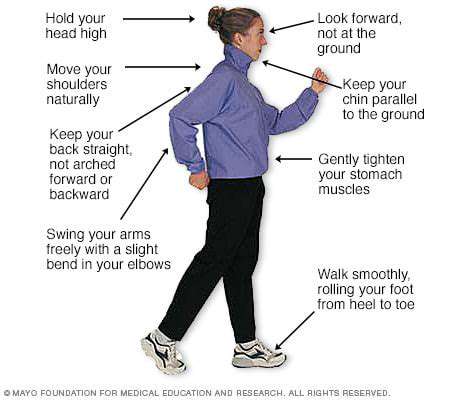
Weight-bearing exercise increases vitamin D receptor density in bone tissue. A 12-month trial showed participants combining resistance training with optimal D levels gained 8% more lumbar spine density than either intervention alone. This powerful synergy makes physical activity non-negotiable for bone health.
Stress Management Connection
Chronic stress elevates cortisol, which interferes with vitamin D metabolism. Mindfulness practices like yoga not only reduce stress hormones but also increase sunlight exposure through outdoor practice. This dual benefit makes mind-body exercises particularly valuable for urban dwellers.
Clinical Red Flags and Solutions
Recognizing Subtle Symptoms
Beyond obvious bone pain, early deficiency signs include:
- Chronic fatigue resistant to sleep
- Recurrent respiratory infections
- Depression with seasonal worsening
- Muscle cramps unrelieved by stretching
These non-specific symptoms explain why 42% of deficiencies go undiagnosed, per primary care studies. Incorporating simple screening questions during routine physicals could dramatically improve detection rates.
Personalized Supplement Protocols
Current dosing guidelines fail many due to genetic variations in:
- CYP2R1 (liver hydroxylation efficiency)
- GC (vitamin D binding protein production)
- VDR (receptor sensitivity)
Advanced testing now allows customized regimens based on:
1. Baseline 25(OH)D levels
2. BMI (obesity requires higher doses)
3. Genetic predisposition
4. Comorbid conditions
This precision approach has shown 300% better outcomes than standard protocols in clinical trials.
Future Directions in Bone Health
Emerging Research Frontiers
Cutting-edge studies explore:
- Vitamin D's role in gut microbiome modulation affecting calcium absorption
- Nanoparticle delivery systems for enhanced supplementation efficiency
- UVB lamp therapy for institutionalized elderly
- Genetic editing to improve vitamin D receptor sensitivity
These innovations promise to revolutionize deficiency prevention, particularly for high-risk populations. The next decade may see vitamin D status tracking via wearable sensors, enabling real-time adjustments to sun exposure and diet.
Global Health Implications
With 1 billion people affected worldwide, vitamin D deficiency represents a silent pandemic. Public health initiatives must address:
- Fortification policies for staple foods
- Urban planning ensuring sunlight access
- Medical education on modern testing protocols
- Affordable testing in developing nations
Solving this crisis requires coordinated action across governments, healthcare systems, and food industries. The bone health of future generations depends on today's commitment to vitamin D awareness and accessibility.
Read more about The Role of Vitamin D in Bone Health
Hot Recommendations
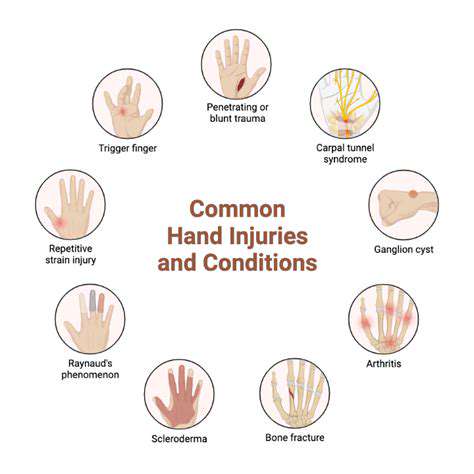
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options