The Role of Physical Therapy in Leg Injury Recovery
Understanding the Importance of Post-Injury Physical Therapy
Physical therapy plays a crucial role in helping patients recover from leg injuries, offering benefits that go well beyond just getting back on your feet. Every rehab plan is customized to fit the injury type, the patient's physical condition, and their personal recovery targets. This tailored method makes sure the healing process works effectively while keeping safety a top priority, helping avoid new problems and ensuring full recovery.
Besides restoring physical function, therapy teaches patients how their body moves and its limits. This knowledge helps people make smarter choices about activities and daily habits, supporting long-term health and preventing future injuries. Proper rehab methods are especially important for lowering the chance of re-injury, which is a major worry after any serious leg trauma.
Addressing Specific Needs of Different Leg Injuries
Rehab methods change significantly based on what kind of leg injury occurred. For instance, recovering from a knee ligament tear follows a different path than healing a shinbone fracture. Therapists carefully evaluate each injury, looking at how severe it is, which tissues were affected, and the patient's particular situation. This detailed assessment is key for building a treatment plan that fits the injury's specific demands.
Therapists also study how patients move, spotting any muscle imbalances or weak areas that might have led to the injury. Finding these issues helps prevent future problems and supports more complete healing. They design exercises to strengthen these weak spots, building up surrounding muscles and improving joint stability. This focused method is vital for full recovery.
Restoring Mobility and Functional Abilities
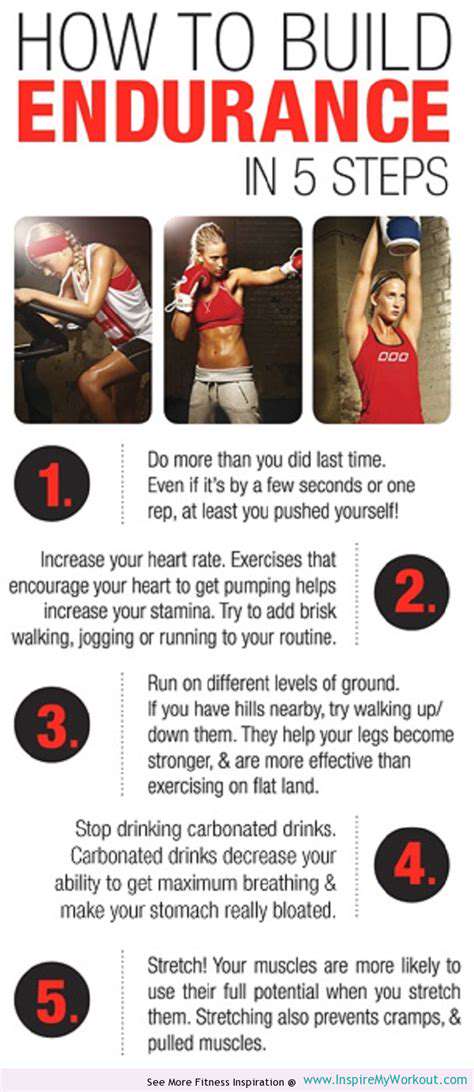
A main focus of post-injury therapy is regaining full movement and everyday abilities. This involves a step-by-step exercise plan, starting with simple motions and slowly increasing difficulty. The exercises are picked to match the injury's limitations, keeping patients challenged but safe. This careful progression helps avoid setbacks and smoothes the return to normal life.
Therapists guide patients through exercises that rebuild strength, flexibility, and stamina. These targeted workouts help restore the leg's ability to handle daily tasks like walking, running, or stair climbing. The therapist tracks progress, adjusting the plan as needed to ensure the best results and safe return to activities.
Long-Term Implications and Preventing Recurrence
Therapy's benefits last well beyond initial recovery; it also helps stop future injuries. By fixing underlying weaknesses or imbalances, therapists give patients the tools to make smart activity choices and develop injury prevention strategies. This forward-thinking approach is key for maintaining health long-term.
Learning proper body mechanics and posture is central to therapy's lasting success. By focusing on these elements, therapists equip patients with knowledge to avoid future injuries, supporting an active, fulfilling life. This emphasis on prevention greatly boosts therapy's overall effectiveness.
Customized Rehabilitation Programs for Effective Leg Injury Management
Individualized Approach
Personalized rehab programs are vital for successful recovery. A plan tailored to the person's needs, goals, and limits works far better than generic solutions. This ensures the program tackles specific challenges and maximizes results.
Since every patient's recovery differs, customized plans allow for gradual progress, adapting to improvements or setbacks to optimize healing.
Comprehensive Assessment
A thorough evaluation forms the foundation of effective rehab. This means checking not just physical issues but also mental health, social factors, and environment. Seeing the full picture of someone's situation is crucial for holistic care.
This assessment pinpoints exactly where help is needed, guiding program development for the best patient outcomes.
Goal Setting and Monitoring
Clear, measurable goals are essential for tracking progress and staying motivated. Goals should be realistic, achievable, and match the patient's long-term hopes. Hitting these targets builds confidence and keeps patients engaged.
Regular progress checks allow for plan adjustments, keeping the program effective and patients focused on their goals.
Exercise Prescription
A well-designed exercise program is rehab's backbone, focusing on strength, flexibility, and endurance. The plan should fit the patient's abilities, gradually increasing difficulty as they improve. This step-by-step approach prevents injury while maximizing gains.
The exercise plan targets the patient's specific needs, preventing setbacks by matching their physical condition.
Therapeutic Techniques
Rehab often uses various techniques like hands-on therapy, heat/cold treatments, and other methods. Choices depend on the injury and patient needs. These approaches help reduce pain, swelling, and restore function.
Patient Education and Support
Teaching patients about their condition is vital for success. When patients understand their situation, treatment plan, and expected results, they become active partners in recovery. This teamwork boosts chances of good outcomes.
Education covers home exercises, self-care, and handling potential problems. Ongoing support from the care team helps maintain progress and prevent relapse.
Interdisciplinary Collaboration
The best rehab programs involve teamwork between physical therapists, doctors, and other specialists. This combined effort ensures all aspects of recovery are addressed. Pooling different experts' knowledge leads to better patient results.
Managing Pain and Swelling Effectively with Physical Therapy Techniques
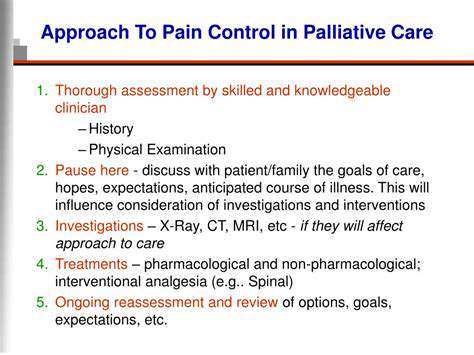
Effective Pain Management Strategies
Therapy offers multiple ways to control pain, focusing on reducing inflammation and promoting healing. Methods include targeted exercises, hands-on therapy, and treatments like heat/ice. By addressing pain's root causes, therapists help patients develop long-term management strategies. This personalized approach considers individual needs, ensuring safe, effective treatment.
A key pain management aspect is understanding how the body reacts to injury. Therapists teach patients about rest, proper posture, and movement to minimize pain and aid healing. They also help identify and avoid pain-triggering activities, empowering patients in their recovery.
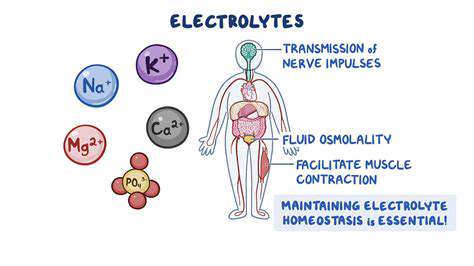
Addressing Swelling with Therapeutic Exercises
Swelling often accompanies injuries, affecting mobility. Therapists use techniques like elevation, compression, and special exercises to reduce it. These exercises improve fluid drainage and circulation, removing excess fluid from injured areas. This targeted approach eases discomfort and speeds healing.
Manual lymphatic drainage, performed by professionals, can be especially effective for swelling. These gentle massages stimulate fluid movement. Combined with exercises, they provide comprehensive swelling management and functional recovery.
Importance of Therapeutic Modalities
Therapists use various treatments to ease pain and promote healing, including heat/cold therapy, ultrasound, electrical stimulation, and laser therapy. Each targets specific body responses like reducing muscle spasms or improving blood flow. Choices depend on patient needs and conditions.
Heat relaxes muscles and boosts circulation, easing pain and stiffness. Cold reduces inflammation and swelling. Combining modalities creates comprehensive plans that optimize recovery and life quality.
Personalized Treatment Plans for Optimal Results
Effective pain/swelling management requires customized plans. Therapists work closely with patients to develop plans matching their needs and goals, considering injury type, medical history, and lifestyle. This ensures safe, effective treatment.
A thorough evaluation comes first, checking movement range, strength, flexibility, and function. Understanding these factors lets therapists create programs that promote healing, reduce pain, and improve wellbeing. This teamwork empowers patients in their recovery journey.
The Long-Term Benefits of Physical Therapy in Preventing Future Injuries

Enhancing Cardiovascular Health
Regular activity is crucial for heart health. Activities like brisk walking, swimming, or cycling strengthen the heart, improving blood pumping efficiency. This lowers blood pressure and cholesterol, reducing heart disease and stroke risk. Consistent exercise also improves blood vessel function, boosting circulation.
Heart health benefits extend beyond disease prevention. A strong heart and healthy vessels ensure proper oxygen/nutrient delivery, supporting energy levels, sleep quality, and brain function.
Boosting Mental Well-being
Exercise benefits both body and mind. Physical activity releases endorphins, natural mood lifters that reduce stress, anxiety, and depression symptoms. This natural boost improves self-esteem and outlook. The accomplishment feeling from regular exercise is empowering.
Activity provides healthy stress relief. Exercise serves as an effective stress manager, improving mental wellbeing. It also enhances sleep quality, vital for mental health.
Strengthening Muscles and Bones
Regular exercise builds muscle and bone strength, improving posture, balance, and function. Weight-bearing activities like walking and dancing increase bone density, reducing osteoporosis risk. This is especially important for maintaining mobility with age.
Strength training builds muscle power and endurance, making daily tasks easier and supporting joints to prevent injury and age-related pain.
Improving Sleep Quality and Longevity
Regular activity significantly improves sleep by regulating natural sleep cycles and reducing fatigue. Better sleep allows proper physical and mental restoration for optimal daily function.
Exercise's positive impact extends lifespan, with studies showing links to reduced chronic disease risk, longer life, and improved quality of life. Building activity into daily routines enhances health prospects for longer, fuller lives.
Read more about The Role of Physical Therapy in Leg Injury Recovery
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health