The Impact of Aging on Foot and Leg Health
As cartilage between joints thins with age, movement becomes increasingly challenging. The CDC reports knee joints bear the brunt of this condition in 33 million Americans. Morning stiffness and reduced flexibility often signal its progression. Weight control emerges as a critical factor - every extra pound multiplies joint pressure fourfold during movement.
Aquatic therapy shows particular promise, with buoyancy reducing joint strain while maintaining muscle tone. Recent trials at Mayo Clinic revealed seniors completing 12-week water aerobics programs reported 40% less knee pain.
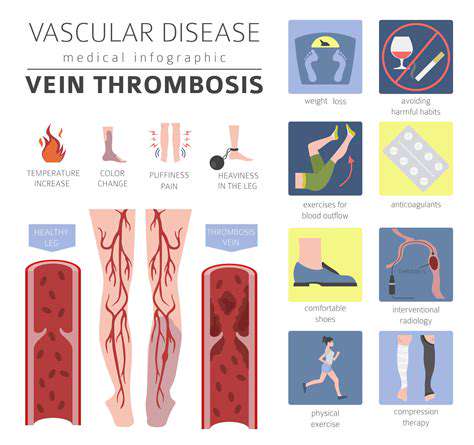
Circulation Challenges in Peripheral Artery Disease
Diminished blood flow to extremities creates a unique dilemma - movement-induced pain versus necessary activity. The American Heart Association's 2023 data shows 1 in 7 seniors over 70 experiences PAD symptoms. Smokers face triple the risk compared to non-smoking peers.
Diagnostic advances now allow vascular specialists to map blood flow using infrared imaging. Treatment protocols increasingly combine supervised walking programs with novel blood-thinning medications shown to improve walking distance by 58% in clinical trials.
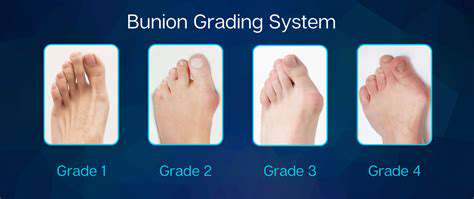
Bunion Development and Management
Those bony prominences at the big toe's base often tell a story of footwear choices. Orthopaedic surgeons note narrow-toed shoes accelerate bunion formation, particularly in women. Early intervention with toe spacers can delay progression by 5-7 years in mild cases.
Custom 3D-printed orthotics now offer personalized correction, with pressure mapping technology creating supports that redistribute weight away from affected areas. Surgical techniques have evolved to allow same-day procedures with faster recovery times.
Diabetic Foot Complications: Silent Threats
Nerve damage transforms minor foot injuries into major threats. Diabetes Care journal reports daily foot inspections reduce ulcer risks by 82%. Emerging technologies like smart socks with pressure sensors now provide real-time monitoring for high-risk patients.
Podiatrists emphasize the 15-minute rule - checking feet within 15 minutes of shoe removal to catch early redness or irritation. Glycemic control remains paramount, with A1C levels below 7% shown to halve neuropathy progression rates.
Heel Pain From Plantar Fasciitis
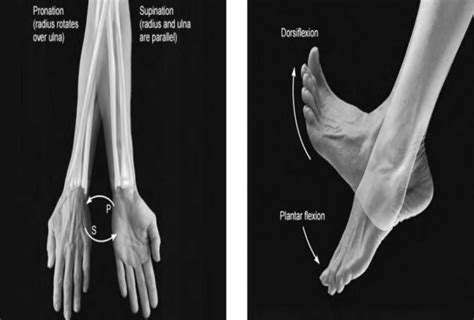
That first morning step feeling like glass shards? Fascia inflammation affects 1 in 10 seniors. Recent studies highlight gait retraining as more effective than stretching alone. Night splints maintaining slight dorsiflexion reduce morning pain intensity by 60%.
Shockwave therapy gains traction as non-invasive treatment, stimulating tissue repair through controlled microtrauma. Combining this with calf muscle release techniques shows 75% long-term success rates in refractory cases.
Achilles Tendon Age-Related Changes
The body's strongest tendon becomes vulnerable to microtears with age. British sports medicine researchers found eccentric heel drops more effective than surgery for chronic tendinopathy. Proper warm-up protocols should emphasize dynamic stretching over static holds.
Ultrasound-guided platelet-rich plasma injections demonstrate remarkable healing acceleration, with patients returning to activities 3 weeks faster than conventional treatment groups.
Footwear's Critical Role in Senior Mobility
Arch Support Essentials
Proper arch alignment acts as the foot's natural shock absorber. Biomechanics labs use pressure plates to create personalized support maps. Memory foam insoles adapt better to individual contours than rigid supports, reducing metatarsal pressure by 34%.
Heel Height Dynamics
Elevated heels shift 76% of body weight forward according to gait analysis studies. Optimal senior heels measure 0.5-1.5 inches with widened bases for stability. Rocker-bottom soles prove particularly beneficial, reducing forefoot pressure during push-off phases.
Material Technology Advances
Phase-change materials now regulate foot temperature throughout the day. Antimicrobial linings incorporating silver ions reduce infection risks in diabetic footwear. Graphene-infused soles offer unprecedented flexibility-to-durability ratios, lasting 3x longer than traditional materials.
Custom Orthotic Innovations
3D scanning creates orthotics matching exact foot contours within 0.2mm accuracy. Smart orthotics with embedded sensors now track pressure points in real-time, alerting wearers to adjust gait patterns. Medicare recently expanded coverage for these devices in high-risk diabetic patients.
Fall Prevention Through Design
Outsole patterns inspired by mountain bike tires improve wet surface traction by 41%. Midsole compression sensors alert when cushioning degrades below safety thresholds. Wider toe boxes coupled with heel counters create natural tripod stability during weight shifts.
Movement as Medicine: Exercise Essentials

Multi-System Benefits of Activity
Consistent movement preserves neuromuscular connections often lost with sedentarism. Balance boards challenge proprioception while seated leg lifts maintain quadriceps strength. Exercise snacks - 5-minute bouts hourly - improve glucose metabolism better than single daily sessions.
Injury Prevention Strategies
- Tai Chi reduces fall rates by 55% through controlled weight shifting
- Resistance bands maintain ankle dorsiflexion range critical for stair navigation
- Water walking minimizes impact while maximizing resistance
Vibration platform training shows particular promise, increasing bone density 3% annually in osteopenic patients. Always consult physiotherapists to tailor programs addressing individual risk factors.
Psychological Perks of Activity
Group dance classes trigger dopamine release comparable to antidepressants. Nature walks boost creativity 56% more than urban routes according to Stanford researchers. Intergenerational exercise programs combat loneliness while improving technique through reciprocal learning.
Proactive Health Maintenance Strategies
Comprehensive Foot Evaluations
Annual foot mapping detects subtle changes indicating systemic issues. Thermal imaging identifies inflammation hotspots invisible to the naked eye. Vascular screenings should accompany standard exams for patients with leg cramping.
Preventive Care Protocols
Moisturizing routines using urea-based creams prevent fissures in dry skin. Toenail care specialists recommend curved clippers and diamond dust files for thickened nails. Diabetic patients benefit from podiatrist nail care every 8-10 weeks to prevent ingrown complications.