Managing Shin Splints in Runners
Comprehensive Interpretation of Shin Splints: A Complete Guide from Prevention to Rehabilitation
Causes and Mechanisms of Shin Splints
Anatomical Perspective of Shin Splints
Shin splints, medically known as medial tibial stress syndrome, primarily manifests as an inflammatory response in the muscles, tendons, and bony structures surrounding the tibia. About 35% of running enthusiasts experience this issue, especially prone to flaring up after suddenly increasing training volume or changing running surfaces. Notably, wearing ill-fitting sports shoes or making sudden changes to running style without a gradual approach can become triggers.
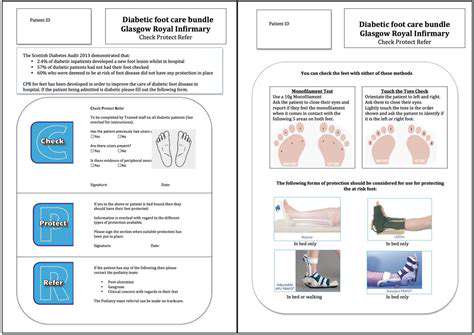
Main Risk Factors Analysis
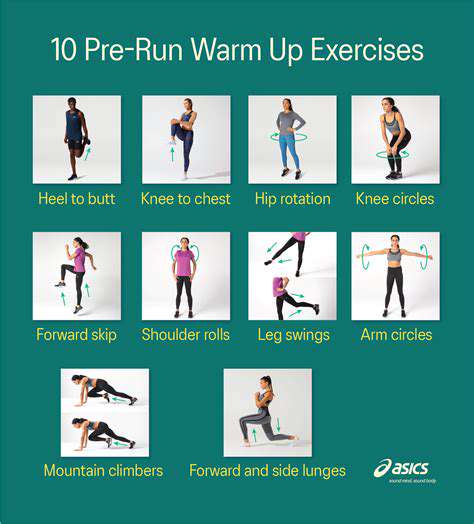
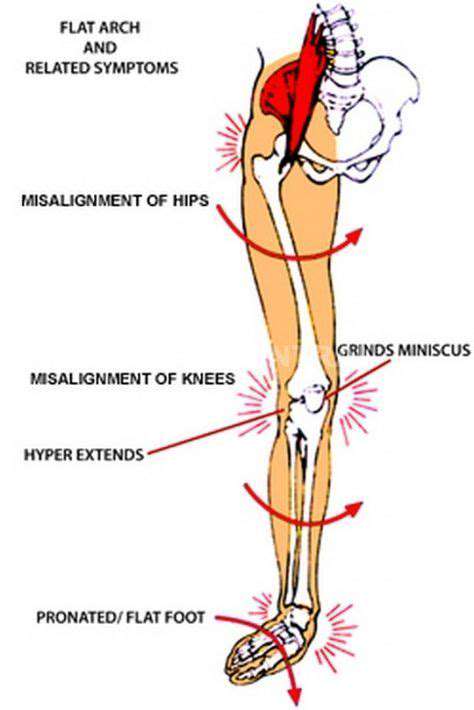
Poor training methods are the most common trigger—such as increasing weekly mileage by more than 10% or insufficient recovery time. Biomechanical abnormalities like excessive foot pronation can significantly increase load on the tibial area, needing special attention to footwear choices for flat-footed or high-arched runners. Recent sports medicine research shows that a systematic dynamic warm-up can reduce the incidence of shin splints by over 40%.
The impact of ground hardness on lower limb shock forces is often underestimated; the reaction force of concrete surfaces can be three times that of a synthetic track. For those with weak calf muscle groups, performing interval training on hard surfaces is akin to planting a time bomb in the tibial area. It is recommended to schedule targeted resistance training twice a week to effectively enhance the cushioning capacity of lower limb muscles.
Identifying Warning Signals of Shin Splints

Typical Symptoms Identification Guide
Patients typically experience progressive pain along the inner edge of the tibia, initially presenting as soreness after exercise, which may develop into persistent dull pain as the condition progresses. About 68% of cases report localized tenderness upon palpation, and in severe cases, even routine walking can cause discomfort. Some patients may also experience slight swelling, which tends to worsen in the evening.
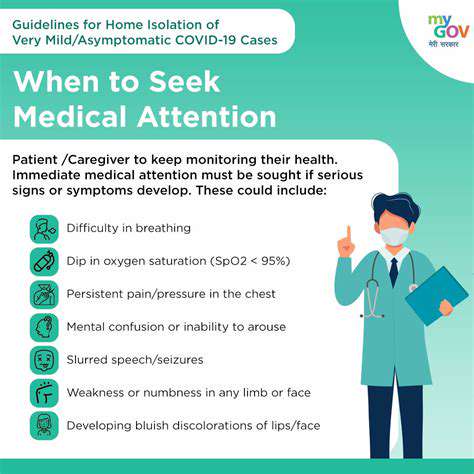
Criteria for Seeking Medical Attention
If self-care has not shown improvement after three weeks, or if there is difficulty standing on one leg, it is essential to seek medical attention promptly. Nights of resting pain are often a sign of a stress fracture and should be confirmed through a bone scan. A professional sports medicine department equipped with gait analysis tools can accurately detect abnormal foot force patterns, which is crucial for formulating a personalized treatment plan.
Systematic Rehabilitation Management Plan
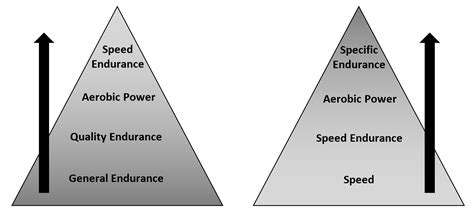
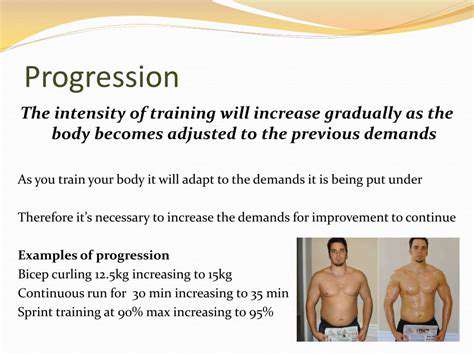
Stepped Training Adjustment Strategy
During the acute phase, complete cessation of running for 2-4 weeks is required, substituting with water running to maintain fitness. In the recovery phase, adhere to the 10-3-1 principle: first complete 10 minutes of brisk walking without pain, followed by a 3-kilometer slow run test, and finally take one week to gradually return to normal training volume. This progressive approach can reduce the recurrence rate by 75%.
The Golden Rule for Footwear Selection
When purchasing running shoes, focus on two parameters: heel drop (recommended 6-8mm) and midsole hardness (recommended 40-60HA). Worn-out shoes can increase foot impact forces by 27%, and they must be replaced once the outsole tread wears down by more than 50%. Custom orthotic insoles can significantly benefit flat-footed patients, effectively dissipating 18%-22% of impact forces.
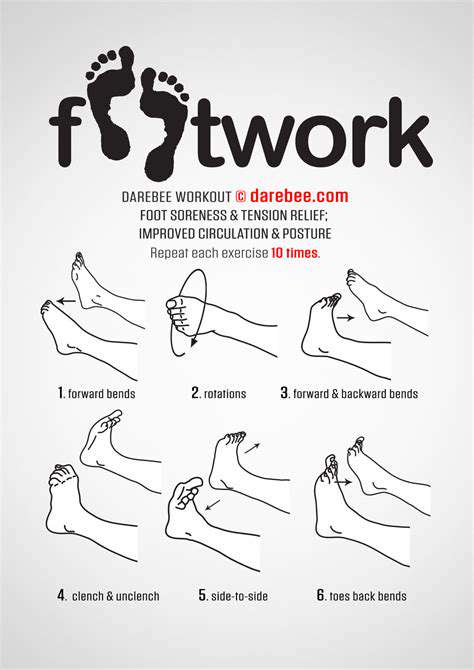
Functional Training Combination Scheme
It is recommended to perform a daily 3+2 training combination: 3 sets of calf raises (20 repetitions per set) combined with 2 minutes of resistance band training. Standing on one leg on a balance pad can significantly enhance proprioception, increasing ankle joint stability by over 40%. When using a foam roller to relax the anterior tibial muscles, maintain pressure on each point for 30 seconds until pain is reduced by 50%.
Building a Long-Term Prevention Mechanism
Digital Management of Training Monitoring
Using a sports watch to record vertical amplitude ratio and ground contact time can effectively reflect running economy. When vertical amplitude exceeds 8.5cm, it indicates excessive landing impact, necessitating timely adjustments to running form. It is advised to conduct a running biomechanics assessment once a month to promptly correct technical flaws.
Three Key Elements of Nutritional Support
Daily supplementation of 1500mg of calcium + 800IU of vitamin D can enhance bone density, and collagen peptides can improve tendon elasticity. Timely post-exercise supplementation with BCAA-containing recovery drinks can accelerate muscle repair processes. These nutritional strategies can reduce the risk of soft tissue injuries by 33%.
Timing for Professional Medical Intervention

Red Alerts to Watch Out For
When experiencing persistent nighttime pain or localized increases in skin temperature, it often indicates the progression of periostitis. Immediate dual-energy X-ray absorptiometry should be conducted to rule out the possibility of stress fractures. Shockwave therapy has shown significant effectiveness for stubborn cases, and combined with eccentric training, it can shorten the rehabilitation cycle by 30%.
Designing Personalized Rehabilitation Plans
Experienced physical therapists will employ the myofascial chain assessment method, conducting a holistic mechanical analysis from the soles of the feet to the lower back. Biomechanical correction plans typically include: hip abductor muscle strengthening (enhancing energy absorption capacity by 17%) + ankle dorsiflexion range of motion training (increasing stride efficiency by 12%). Such comprehensive interventions can reduce the recurrence rate to below 15%.
Read more about Managing Shin Splints in Runners
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options