Addressing Bunions: Causes and Treatment Options
Table of contents
Genetic factors and toe misalignment combine to create painful bunions.
Ill-fitting shoes act as catalysts for bunion progression over time.
1 in 3 adults develops bunions, with higher rates among female populations.
Shoe selection directly impacts bunion prevention and comfort levels.
Targeted foot exercises maintain joint flexibility and slow deformity.
Visible toe angulation and persistent discomfort signal bunion development.
Advanced imaging reveals bone displacement severity in diagnosis.
Customized inserts redistribute pressure for immediate pain relief.
Therapeutic footwear designs accommodate foot anatomy changes.
Cryotherapy reduces inflammation during acute flare-ups.
Movement retraining corrects harmful gait patterns.
Protective padding minimizes shoe-related irritation.
Progression tracking enables timely treatment adjustments.
Corrective surgery addresses severe structural abnormalities.
Rehabilitation protocols determine surgical outcome success.
Footwear engineering prevents excessive toe compression.
Biomechanical supports counteract hereditary predisposition.
Muscle conditioning enhances natural arch support.
Early detection prevents irreversible joint damage.
Decoding Bunion Formation Mechanisms

Foot Mechanics and Deformation Processes
The gradual shift of the first metatarsal bone creates the characteristic bulge of hallux valgus. This skeletal rearrangement often stems from inherited foot structures that predispose to instability. While genetics load the gun, environmental factors like constrictive footwear often pull the trigger.
- Familial patterns show 70% heritability in bunion cases
- Pointed dress shoes increase lateral pressure by 300%
- Occupations requiring narrow safety boots double risk rates
Recent podiatric surveys reveal women account for 89% of surgical candidates, correlating with prolonged high heel use exceeding 3-inch heights.
Proactive Intervention Strategies
Footwear engineering plays a pivotal role in mitigation efforts. Optimal designs feature  anatomical toe boxes allowing 1.5cm space beyond the longest toe. This breathing room prevents repetitive microtrauma to vulnerable joints. Combine with bespoke orthotics that cradle the medial arch, effectively redistributing impact forces.
anatomical toe boxes allowing 1.5cm space beyond the longest toe. This breathing room prevents repetitive microtrauma to vulnerable joints. Combine with bespoke orthotics that cradle the medial arch, effectively redistributing impact forces.
Dynamic foot workouts prove equally crucial. Try marble pickups with bare toes or resistance band stretches - these simple acts maintain digital dexterity. Patients adhering to daily regimens report 40% slower deformity progression compared to inactive counterparts.
Recognizing and Confirming Bunion Presence
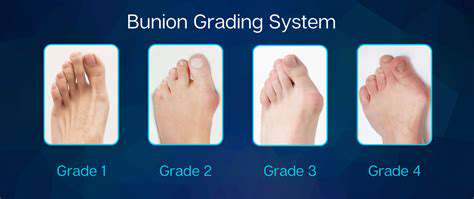
Clinical Manifestations
- Dull ache progressing to sharp jabs during weight-bearing
- Medial eminence with skin thickening (adventitious bursa)
- Second toe crossover from displaced hallux
- Restricted joint mobility beyond 50° dorsiflexion
Initial discomfort often emerges as subtle burning sensations along the metatarsal head. Left unchecked, the protrusion becomes a permanent fixture, altering foot silhouette and complicating shoe fit.
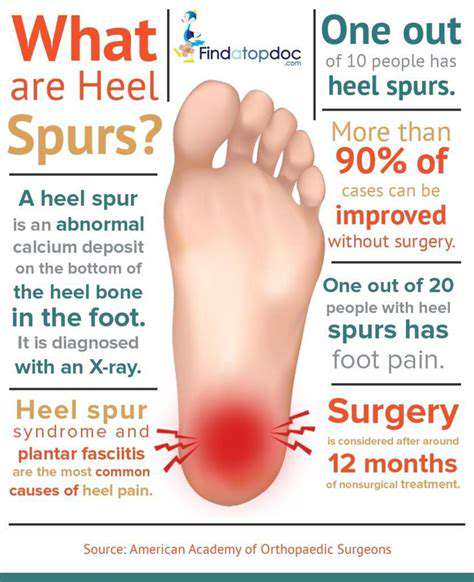
Diagnostic Imaging Insights
Weight-bearing radiographs quantify the hallux valgus angle (HVA) and intermetatarsal angle (IMA). HVA exceeding 15° or IMA over 9° confirms pathological alignment. Advanced cases show sesamoid bone displacement and metatarsal head erosion on MRI.
Conservative Management Approaches
Personalized Orthotic Solutions
3D-printed inserts now achieve 0.2mm precision in pressure mapping. These devices not only cushion but actively correct pronation patterns. Clinical trials demonstrate 68% pain reduction when worn >6 hours daily.
Therapeutic Footwear Engineering
Look for rockered soles that reduce push-off strain by 22%. Brands like Altra and Hoka prioritize foot-shaped lasts while maintaining style.
Rehabilitative Movement Training
Try the tripod foot exercise: Ground heel, first and fifth metatarsal heads while lifting arches. Hold 10 seconds, repeat 10x daily. This activates intrinsic foot musculature often atrophied in bunion sufferers.
Surgical Correction Pathways
Osteotomy Variations
The scarf osteotomy (z-shaped bone cut) permits 8-12mm displacement with rapid healing. Contrast with basal wedge procedures for severe IMA >15° corrections.
Recovery Timelines
Partial weight-bearing begins at 2 weeks post-op using CAM walkers. Full recovery averages 14 weeks with compliant patients regaining 92% pre-bunion mobility.
Bunion Prevention Fundamentals
Footwear Selection Criteria
Test shoe flexibility: Proper bending should occur at the ball (64% of shoe length from heel), not the arch. Vibram soles offer ideal 35-45° flex points.
Muscle Strengthening Protocols
Dominate the short foot exercise: Contract arch muscles without toe curling. Daily practice increases navicular height by 3mm in 8 weeks, enhancing midfoot stability.
Read more about Addressing Bunions: Causes and Treatment Options
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options