The Impact of Diabetes on Hand Health
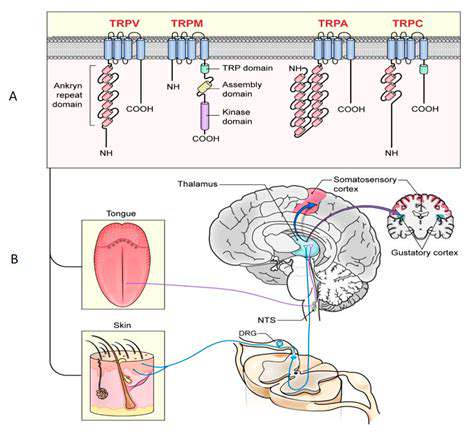
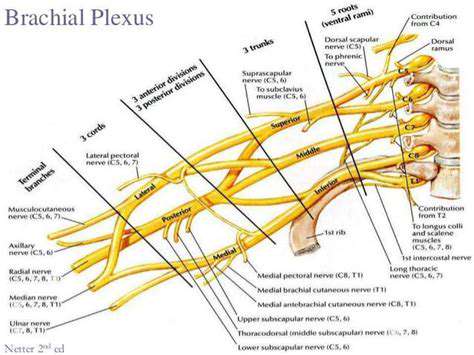
Peripheral neuropathy is a debilitating condition that affects the nerves outside of the brain and spinal cord. It often develops gradually, making it difficult to recognize the early warning signs. This insidious nature of the disease can lead to significant delays in diagnosis and treatment, potentially exacerbating the symptoms and hindering recovery.
The condition can manifest in a variety of ways, from mild discomfort to severe pain, numbness, and tingling. Understanding the different forms of peripheral neuropathy and their associated symptoms is crucial for early detection and appropriate intervention.
Causes and Risk Factors
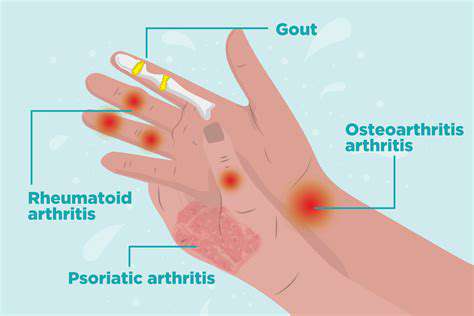
Peripheral neuropathy can arise from a multitude of underlying causes, including diabetes, infections, nutritional deficiencies, autoimmune disorders, and certain medications. Diabetes is a particularly significant risk factor, frequently leading to nerve damage due to high blood sugar levels. Identifying the root cause is vital for developing an effective treatment strategy.
Other factors, such as alcohol abuse, kidney disease, and exposure to toxins, can also increase the risk of developing peripheral neuropathy. Understanding these risk factors can help individuals take proactive steps to mitigate their chances of developing the condition.
Symptoms and Diagnosis
Recognizing the symptoms of peripheral neuropathy is crucial for seeking timely medical attention. Symptoms can range from mild numbness or tingling in the extremities to intense pain, weakness, and difficulty with balance. Early diagnosis is often challenging due to the subtle nature of some symptoms.
A comprehensive neurological evaluation, including physical examination, nerve conduction studies, and electromyography, is often necessary to diagnose peripheral neuropathy. These tests help determine the specific type and extent of nerve damage.
Treatment Options
Treatment for peripheral neuropathy focuses on managing the underlying cause and alleviating symptoms. This may involve medication to control pain, manage blood sugar levels, or address the underlying autoimmune disorder. Effective management often requires a multidisciplinary approach, incorporating physical therapy, occupational therapy, and lifestyle modifications.
Living with Peripheral Neuropathy
Living with peripheral neuropathy can be challenging, requiring significant adjustments to daily life. Adapting to pain, discomfort, and potential mobility issues is often a significant hurdle. Support groups and educational resources can provide valuable assistance and information to manage the condition effectively.
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques, plays a crucial role in improving overall well-being and managing symptoms.
Seeking Expert Care and Support
Understanding the Diabetic Neuropathy Connection
Diabetic neuropathy, a common complication of diabetes, significantly impacts the hands. It stems from damage to the nerves in the hands and throughout the body. This damage can lead to a multitude of symptoms, including reduced sensation, numbness, and pain. Often, individuals with diabetic neuropathy experience a gradual loss of feeling in their hands, making it difficult to detect minor injuries or temperature changes. This diminished awareness can lead to more serious problems if not carefully managed.
The impact of this nerve damage extends beyond simple discomfort. It can impair fine motor skills, making everyday tasks, like buttoning clothes or handling small objects, challenging. The progressive nature of diabetic neuropathy means that symptoms can worsen over time, requiring proactive strategies for prevention and management.
The Role of Poor Circulation in Hand Health
Diabetes can also negatively affect blood circulation, particularly in the extremities like the hands. Reduced blood flow restricts the delivery of essential nutrients and oxygen to the tissues in the hands. This can result in a variety of issues, from persistent coldness and tingling to a slower healing process of cuts and sores. The combination of reduced sensation and poor circulation creates a dangerous environment for hand injuries, potentially leading to infections and ulcers.
Maintaining healthy blood sugar levels, along with regular exercise and a balanced diet, are crucial for improving circulation and reducing the risk of complications. Seeking professional advice on managing these circulation issues is essential for safeguarding hand health and overall well-being.
Preventive Measures and Expert Intervention
Proactive steps are vital in preventing further damage to hand health. Regular foot and hand exams by healthcare professionals are crucial for early detection of potential problems. These exams allow for prompt intervention to address any developing issues, such as ulcers or infections. Diligent self-care, including meticulous hand hygiene and prompt treatment of any cuts or abrasions, is equally important. Taking preventative measures, combined with expert intervention when needed, can significantly reduce the long-term impact of diabetes on hand health.
Working with a healthcare team, including a podiatrist or hand specialist, is essential for developing a personalized care plan. This plan may incorporate specialized footwear, hand exercises, or other therapies to alleviate symptoms and prevent further complications. By actively participating in preventive care and seeking expert guidance, individuals with diabetes can significantly improve their hand health and maintain a higher quality of life.