The Impact of Aging on Hand Function
The Spectrum of Sensory Changes
Sensory disturbances following nerve damage vary tremendously between individuals. Some experience the classic pins and needles sensation, while others report more bizarre symptoms like feeling water droplets that aren't there. Perhaps most concerning is the loss of protective sensation, where individuals can't feel injuries occurring. This explains why diabetics might only discover foot ulcers during routine checks.
The location of nerve damage creates distinct symptom patterns. Carpal tunnel syndrome typically affects just three fingers, while cervical radiculopathy might alter sensation across an entire arm. Temperature perception often disappears before light touch, creating situations where burns occur without pain signals. These graduated losses complicate self-protection efforts.
Evaluating Neurological Function
Modern neurology employs sophisticated tools to map nerve damage, but the diagnostic process still begins with simple clinical tests. A tuning fork applied to bony prominences can reveal vibration sense deficits long before advanced imaging shows changes. Two-point discrimination tests using calipers help quantify tactile resolution - crucial for hand function assessment.
Electrodiagnostic studies provide objective data, but interpreting results requires expertise. Nerve conduction velocities slow with age naturally, so comparing against age-matched norms becomes essential. Skin biopsy for intraepidermal nerve fiber density now offers a direct measure of small fiber neuropathy, particularly useful for diagnosing mysterious pain syndromes.
Comprehensive Treatment Approaches
Effective management requires addressing both the nerve damage and its functional consequences. For traumatic injuries, timely surgical intervention can mean the difference between recovery and permanent disability. Microsurgical techniques now allow reconnection of nerves with precision unimaginable just decades ago. Meanwhile, medication regimens must balance symptom control against side effects - gabapentin may help neuropathic pain but often causes drowsiness.
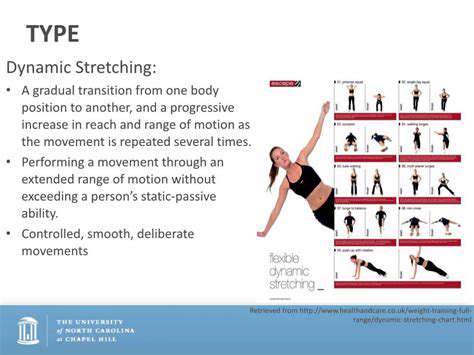
Occupational therapists play a crucial role in retraining the brain to interpret altered sensory input. Mirror therapy has shown promise for phantom limb pain, while sensory re-education programs help stroke survivors regain hand function. Adaptive equipment, from weighted utensils to textured grips, can maintain independence despite sensory deficits.
Practical Strategies for Hand Health
The Aging Hand: What Changes and Why
Hands tell the story of a lifetime's use. Joint capsules thicken, cartilage wears thin, and tendons lose elasticity - all part of normal aging. But these changes accelerate with certain activities. Years of typing with improper wrist alignment or manual labor with vibrating tools leave their mark. Interestingly, dominant hands often show more severe changes, demonstrating the impact of cumulative use.
Microscopically, aging hands lose Meissner's corpuscles - the touch receptors concentrated in fingertips. This explains why older adults struggle with fine manipulations like buttoning shirts or threading needles, even when muscle strength remains adequate.
Ergonomics in Daily Life
Modern technology presents both challenges and solutions for hand health. Voice-to-text software reduces typing demands, while ergonomic keyboards maintain neutral wrist positions. The key principle: avoid sustained positions at joint extremes. When using handheld devices, alternate hands frequently and take microbreaks every 15 minutes.
In the kitchen, consider tool modifications. Rocker knives require less grip force, while jar openers with extended handles provide better leverage. Even simple changes like using a curved shower brush can prevent shoulder strain that indirectly affects hand positioning.
Targeted Hand Exercises
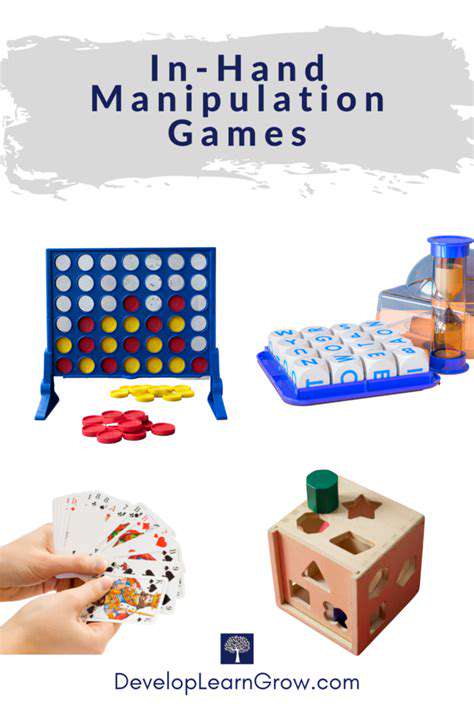
Effective hand conditioning goes beyond simple squeezes. Try the coin pick-up exercise: place various coins on a table and practice retrieving them using different finger combinations. For dexterity, practice rotating a pencil between fingers like a baton. These functional exercises mimic real-world tasks while improving coordination.
Don't neglect wrist and forearm conditioning - their strength directly impacts hand function. Reverse wrist curls with light weights (1-2 lbs) help prevent tendinitis. For arthritis sufferers, warm paraffin wax treatments before exercise can reduce stiffness and pain.
Nutritional Support for Connective Tissue
Emerging research highlights specific nutrients for tendon and ligament health. Hydrolyzed collagen peptides show promise for improving joint comfort, particularly when combined with vitamin C. Omega-3 fatty acids from fish oil may reduce inflammatory processes that degrade joint tissues.
Antioxidant-rich foods combat oxidative stress that accelerates connective tissue aging. Tart cherry juice contains anthocyanins that may ease joint discomfort, while ginger's anti-inflammatory properties could benefit those with hand arthritis.
Early Warning Signs
Subtle symptoms often precede major hand problems. Morning stiffness lasting less than 30 minutes may suggest early osteoarthritis. Difficulty turning doorknobs or car keys could indicate emerging thumb base arthritis. Even changes in handwriting - larger, less precise letters - may reflect declining fine motor control.
Protective Measures
Environmental protection goes beyond obvious hazards. Cold weather particularly stresses arthritic joints - consider heated gloves for winter outings. UV protection matters too; the thin skin on hands shows sun damage quickly. Look for gloves with UPF ratings for extended outdoor activities.
For hobbyists, vibration-dampening tools protect against white finger syndrome. Gardeners should choose pruners with rotating handles to reduce repetitive strain. Even smartphone users can benefit from styluses that reduce thumb overuse.