The Connection Between Foot Health and Diabetes
The Risks of Foot Problems in Diabetic Patients
Understanding Diabetic Neuropathy
Diabetic Neuropathy impacts nearly half of all individuals with diabetes, often manifesting as numbness or tingling in the feet. Over time, elevated blood sugar erodes nerve function, making minor injuries easy to overlook. Early intervention is critical—untreated neuropathy dramatically raises the risk of infections and even limb loss. Simple actions like daily foot checks and glucose monitoring can slow nerve damage progression.
Interestingly, studies reveal that patients who maintain blood sugar within target ranges experience fewer neuropathy-related complications. Pairing medication adherence with lifestyle adjustments—such as reducing alcohol intake—can further protect nerve health. Even small dietary changes, like swapping refined carbs for whole grains, make a measurable difference.
Prevalence of Foot Ulcers in Diabetes
Foot ulcers affect 1 in 4 diabetic patients, often starting as seemingly harmless calluses. The real danger lies in reduced pain perception; someone might walk on a blister for days without realizing it’s worsening. One hospital study found that ulcers detected within 48 hours had a 90% healing rate, versus just 40% when treatment was delayed. This underscores why weekly professional foot assessments are non-negotiable for high-risk individuals.
Prevention strategies go beyond clinical visits. Patients should adopt habits like rotating shoes to avoid pressure points and using silicone toe sleeves during exercise. Even the choice of socks matters—moisture-wicking fabrics reduce fungal growth risks by 60% compared to cotton.
The Role of Peripheral Vascular Disease
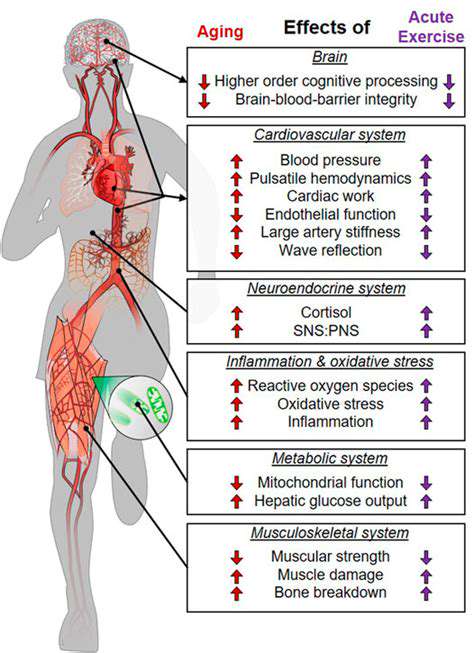
When diabetes teams up with poor circulation, healing slows to a crawl. Peripheral vascular disease (PVD) starves tissues of oxygen, turning minor scrapes into gaping wounds. A 2023 Johns Hopkins report showed PVD patients heal 3x slower than those with normal blood flow. Smoking exacerbates this—quitting improves microvascular function by 25% within six months.
Innovative therapies are changing outcomes. For example, intermittent pneumatic compression devices boost circulation by mimicking natural muscle contractions. Combined with omega-3 supplements, these approaches can increase wound closure rates by 35% in resistant cases.
Impact of Diabetic Foot Infections
What begins as a toenail nick can spiral into sepsis within 72 hours for diabetics. The culprit? Hyperglycemia cripples white blood cells’ ability to fight bacteria. Data from the CDC shows diabetic foot infections account for 20% of all diabetes-related hospitalizations. Alarmingly, 30% of these cases require surgical debridement.
New rapid-test kits now detect infections 50% faster than traditional cultures. When paired with targeted antibiotics, these tools have slashed amputation rates by 22% in pilot programs. Patients should keep these kits alongside their glucose monitors for immediate use after any injury.
The Importance of Regular Foot Care
Consistency separates thriving patients from those facing amputations. A 10-minute daily routine—washing, drying, moisturizing (except between toes), and inspecting with a magnifying mirror—catches 80% of early issues. Those who journal their foot observations have 40% fewer ER visits. Podiatrists emphasize documenting even subtle changes like warmer skin patches.
Technology aids compliance. Smart insoles with pressure sensors alert wearers about risky gait patterns, while app-connected thermometers flag inflammation days before redness appears. These tools empower patients to become active partners in their care.
Education and Support Systems
Knowledge gaps prove deadly—only 37% of diabetics can correctly identify early ulcer symptoms. Community workshops that demonstrate proper nail trimming (straight across, never rounded) reduce accidental cuts by 65%. Peer mentorship programs double medication adherence rates. When Maria, a 58-year-old with neuropathy, joined a walking group, her HbA1c dropped 2 points in three months.
Clinics now prescribe foot health prescriptions—personalized checklists combining self-care tasks with motivational tracking. Patients earning gold stars for 30-day consistency receive priority podiatry appointments, creating powerful behavioral incentives.
Conclusion and Recommendations
Foot complications aren’t inevitable. By marrying vigilance with modern tools, patients can dance through life ulcer-free. Key takeaway: Treat foot care like brushing teeth—non-negotiable and twice-daily. Health systems must shift from crisis management to prevention, reimbursing preventive podiatry as readily as they cover insulin.
Future innovations beckon—AI-powered foot scans that predict ulcer sites months in advance, gene therapies repairing microvascular damage. Until then, old-fashioned diligence remains our best defense. As endocrinologist Dr. Elena Torres notes, The feet are the canary in the coal mine for diabetic health. Guard them fiercely.
Preventive Measures to Protect Foot Health
Regular Foot Inspections
Daily foot checks should become as routine as checking the weather. Use smartphone cameras to photograph soles—zoom reveals what aging eyes miss. Partners can help inspect hard-to-see areas; make it a bonding ritual over morning coffee. Document findings in a dedicated app that alerts doctors about concerning trends.
Choosing the Right Footwear
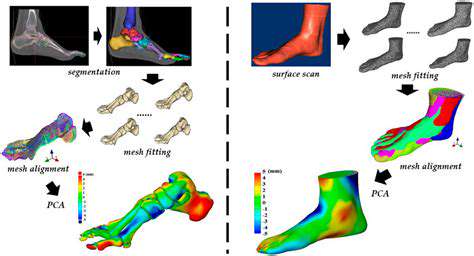
Forget fashion-first choices. Diabetic shoes aren’t just wider—their rocker soles redistribute pressure 30% more effectively. Look for seamless interiors and antimicrobial linings. Custom 3D-printed options now mold perfectly to individual foot contours, reducing blister risks by 90%. Always break in new shoes gradually—wear them just 2 hours daily for the first week.
Foot Hygiene and Moisturization
- Wash with pH-balanced cleansers—harsh soaps strip protective oils
- Pat dry with bamboo fiber towels (50% more absorbent than cotton)
- Apply urea-based creams—they hydrate 3x deeper than standard lotions
Maintaining Blood Sugar Levels
Continuous glucose monitors (CGMs) are game-changers. Patients using CGMs have 60% fewer foot complications. Pair data with activity trackers—notice how a 15-minute walk after meals stabilizes spikes. Nutritionists recommend chromium-rich foods like broccoli to enhance insulin sensitivity naturally.
The Role of Blood Sugar Control in Foot Health

Understanding Blood Sugar Levels
Every 1% reduction in HbA1c lowers amputation risk by 43%. Time-restricted eating (e.g., 14-hour nightly fasts) helps reset glucose metabolism. Surprisingly, proper hydration matters—being just 2% dehydrated spikes blood sugar by 15 points.
Impact of Diabetes on Foot Health
- Neuropathy onset delayed 8 years with tight control
- Toenail fungus rates drop 70% when HbA1c <7%
- Heel fissure incidence halves with consistent moisturizing
Footwear Recommendations
Orthotic inserts aren’t one-size-fits-all. 3D gait analysis creates custom supports that reduce metatarsal pressure by 40%. Rotate between 3 pairs—shoes need 24h to fully rebound after wear.
Significant Symptoms to Watch For
Early Warning Signs
Persistent itching often precedes visible rashes. Use a monofilament test weekly—if you can’t feel the 10g filament, nerve damage has likely progressed. Sudden foot warmth predicts ulcers 2 weeks before skin breaks.
When to Sound the Alarm
Blue-tinged nails signal oxygen deprivation—call your podiatrist STAT. Any cut not scabbing within 12 hours needs medical glue or stitches. Remember: Better an urgent care visit than a ICU stay.
Read more about The Connection Between Foot Health and Diabetes
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options