Signs of Nerve Damage in the Arm

Identifying the Initial Signs
Pinpointing the very first symptoms of a medical condition is crucial for early diagnosis and effective treatment. Often, these initial signs are subtle and easily overlooked, leading to delayed intervention. Understanding what to look for, even seemingly minor changes in your body, can significantly impact the outcome. By meticulously observing and documenting these early warning signals, you can empower yourself and your healthcare provider to make informed decisions.
Early detection is critical, and recognizing subtle changes is key. While some symptoms are dramatic and obvious, many others present as gradual shifts in your well-being. These subtle changes may include fatigue, mild aches, or unusual sleep patterns. It's important to remember that these initial symptoms, while seemingly insignificant, can provide valuable clues about potential underlying issues.
Categorizing Symptoms by System
A systematic approach to symptom identification is often beneficial. Grouping symptoms based on the body system they affect can help narrow down potential causes. For instance, respiratory symptoms like coughing or shortness of breath might point to a lung-related problem, while digestive issues like abdominal pain or nausea could indicate a gastrointestinal issue. This categorization process can significantly streamline the diagnostic process.
Understanding how different body systems function can provide valuable context for interpreting symptoms. This knowledge allows you to better understand the potential relationships between various physical sensations and their possible causes. By linking symptoms to specific systems, you can significantly improve the efficiency and accuracy of medical investigations. This is a crucial step in determining the appropriate course of action and facilitating effective communication with healthcare professionals.
Recognizing patterns and correlations within these systems can also be highly informative. The presence of multiple symptoms related to a particular system may suggest a more serious condition requiring immediate attention.
Considering Severity and Duration
The severity and duration of symptoms are also vital factors in understanding their significance. A mild headache lasting a few hours is likely less concerning than a severe headache accompanied by nausea and lasting several days. Careful consideration of these factors can help distinguish between common ailments and more serious conditions.
The duration of a symptom can be a crucial indicator. A short-lived symptom, such as a fleeting rash, may be a minor reaction or an allergic response. Conversely, a persistent symptom, such as persistent cough, warrants further investigation.
Assessing Associated Factors
Beyond the symptoms themselves, consider other relevant factors. These factors can include your overall health status, recent illnesses or exposures, and any medications you are currently taking. All of these factors can impact how your body reacts to certain stimuli or conditions.
Family history, lifestyle choices, and environmental exposures are also important contributing factors. These contextual elements can provide valuable insights into the potential causes of your symptoms and guide the diagnostic process. For instance, a family history of heart disease might increase the likelihood of certain cardiovascular symptoms requiring immediate attention.
Lifestyle choices and environmental influences play a substantial role in symptom development. Smoking, poor diet, or exposure to toxins can significantly impact your health and contribute to specific symptoms.
Exploring the Impact on Motor Function: Muscle Weakness and Loss of Coordination
Muscle Weakness: A Comprehensive Overview
Muscle weakness, a common symptom in various conditions, significantly impacts motor function. It's characterized by a reduced ability to generate force, leading to difficulties in performing everyday tasks like walking, lifting objects, or even simple movements such as raising an arm. This decline in strength can stem from a multitude of factors, including nerve damage, muscle diseases, or even nutritional deficiencies. Understanding the underlying causes is crucial for effective treatment and management of this debilitating condition.
The manifestation of muscle weakness can range from subtle difficulties to complete inability to move. This variability necessitates careful assessment and diagnosis to pinpoint the root cause. Factors such as the location and pattern of weakness, associated symptoms, and medical history all contribute to the diagnostic process. Identifying the specific cause allows for targeted interventions that can help restore strength and improve quality of life.
Loss of Coordination: Deviations from Smooth Movement
Loss of coordination, also known as ataxia, is another crucial aspect of impaired motor function. It manifests as a disruption in the smooth and controlled execution of movements. This can result in clumsiness, stumbling, and difficulty with balance. Individuals experiencing ataxia may struggle with tasks demanding precision and dexterity, such as writing, eating, or using utensils.
Several neurological conditions can contribute to ataxia, including stroke, multiple sclerosis, and certain inherited disorders. The specific type and severity of ataxia can vary depending on the underlying cause, impacting the individual's ability to perform activities of daily living. Recognizing the symptoms and seeking appropriate medical attention is essential for managing the condition and mitigating its impact on daily life.
Underlying Causes and Contributing Factors
Various factors can contribute to muscle weakness and loss of coordination, ranging from relatively benign conditions to severe and potentially life-threatening illnesses. These include nutritional deficiencies, such as vitamin D or potassium, which can affect muscle function. Moreover, certain medications, especially those used to treat chronic conditions, can have adverse effects on muscle strength and coordination.
Neurological disorders, including spinal cord injuries, peripheral neuropathies, and stroke, are among the primary causes of motor dysfunction. These conditions disrupt the communication pathways between the brain and muscles, leading to diminished strength and impaired coordination. In addition, certain autoimmune diseases, such as myasthenia gravis, directly target the neuromuscular junction, further exacerbating muscle weakness and loss of coordination. The precise cause of these issues often requires comprehensive medical evaluation.
Diagnosis and Treatment Approaches
Accurate diagnosis is crucial for effectively managing muscle weakness and loss of coordination. This typically involves a thorough medical history, physical examination, and often, specialized tests like nerve conduction studies and electromyography. These assessments help pinpoint the underlying cause of the motor impairment and guide the appropriate treatment strategy.
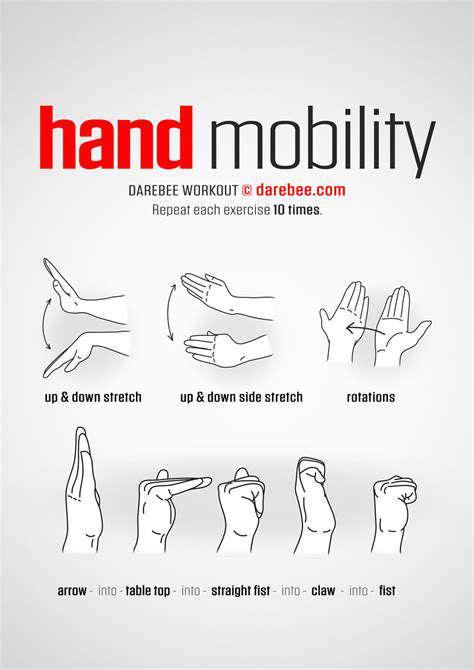
Treatment approaches vary significantly depending on the root cause. Physical therapy, occupational therapy, and medication are common interventions. Physical therapy focuses on restoring strength, improving balance, and enhancing coordination through targeted exercises and rehabilitation programs. Occupational therapy helps adapt daily tasks and environments to accommodate the limitations imposed by muscle weakness and loss of coordination. Medications might be prescribed to address specific conditions contributing to the impairments.
Before you even think about lighting the oven, meticulous preparation is key to a delicious roast. This involves more than just seasoning the meat; it's about understanding the cut of meat you're working with and adjusting your cooking methods accordingly. Properly seasoning the meat, whether it's with herbs, spices, or a simple salt and pepper blend, is crucial for enhancing its natural flavors. You should also consider the size and thickness of the roast, as these factors will significantly impact the cooking time and temperature.
Potential Causes of Arm Nerve Damage: From Injuries to Underlying Conditions
Nerve Compression
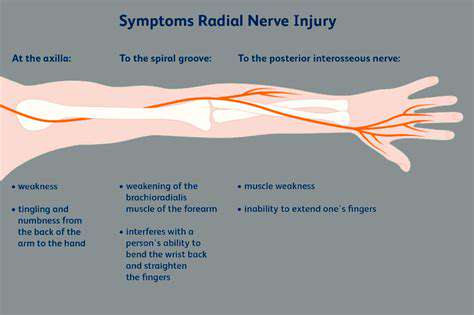
Nerve compression, often stemming from repetitive motions or sustained pressure on the nerves in the arm, can lead to a variety of symptoms. This can manifest in various ways, from mild discomfort to more severe pain, numbness, and tingling. Understanding the specific movements or postures that exacerbate these symptoms is crucial for proper diagnosis and treatment. A thorough examination by a healthcare professional is essential to pinpoint the exact location and cause of the compression.
Carpal tunnel syndrome, a common example of nerve compression, results from pressure on the median nerve within the wrist. This can cause numbness and tingling in the thumb, index, middle, and ring fingers. Early intervention is often key to managing the condition effectively and preventing further damage. Proper ergonomic practices, splinting, and physical therapy can all play a significant role in alleviating symptoms and potentially reversing the damage.
Other potential sources of nerve compression in the arm include conditions like ulnar nerve entrapment at the elbow (cubital tunnel syndrome) and thoracic outlet syndrome, which affects nerves and blood vessels in the upper chest and shoulder area. Each of these conditions presents unique symptoms and requires tailored diagnostic and treatment approaches.
Traumatic Injuries
Trauma to the arm, such as fractures, dislocations, or penetrating wounds, can directly damage nerves. The severity of the injury can range from minor bruising to complete nerve severance. Prompt medical attention is critical to minimizing the potential for permanent nerve damage. Early diagnosis and treatment can significantly improve outcomes, potentially restoring function and alleviating pain.
Surgical intervention may be necessary in cases of severe nerve damage, aiming to repair or re-route the affected nerves. Rehabilitation and physical therapy are essential components of the recovery process to regain strength, coordination, and range of motion in the affected arm.
Sports injuries, falls, and accidents involving the arm can all lead to traumatic nerve damage. Understanding the mechanism of injury is essential for accurate diagnosis and appropriate treatment. The specific type of nerve damage and the extent of the injury will influence the course of treatment and recovery period.
In addition to direct trauma, repetitive stress injuries can also lead to nerve damage. Chronic strain on the nerves in the arm over time can result in inflammation and compression, eventually leading to nerve dysfunction.
Read more about Signs of Nerve Damage in the Arm
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health