Managing Neuropathy in the Feet
Seeking Support and Professional Guidance
Understanding the Underlying Causes
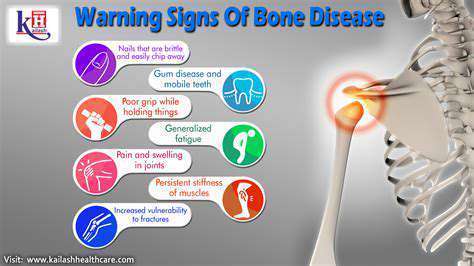
Neuropathy in the feet can stem from a variety of factors, ranging from diabetes and nerve damage to vitamin deficiencies and certain infections. Identifying the root cause is crucial for developing an effective management plan. A thorough medical evaluation is essential to pinpoint the specific type of neuropathy and its contributing factors. This involves a comprehensive history, physical examination, and potentially diagnostic tests to determine the severity and extent of the nerve damage.
Diabetes, for example, is a significant risk factor, often leading to peripheral neuropathy. High blood sugar levels over time can damage the nerves in the extremities, including the feet. Other causes might include autoimmune disorders, alcohol abuse, or exposure to toxins. Accurately diagnosing the underlying cause will guide appropriate treatment strategies.
Managing Pain and Discomfort
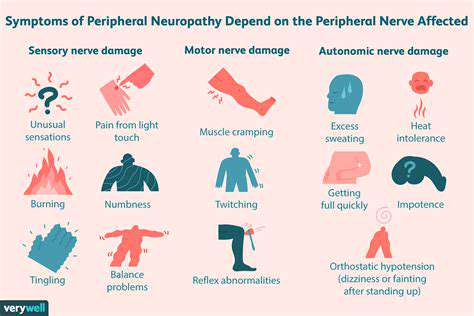
Foot neuropathy often manifests as pain, numbness, tingling, and burning sensations. Managing these symptoms effectively is a key aspect of overall care. Over-the-counter pain relievers might provide some relief, but more potent medications may be necessary in severe cases. A healthcare professional can recommend appropriate pain management strategies, balancing medication with lifestyle adjustments and other therapies.
Understanding the triggers for pain flares is also essential. Certain activities, footwear, or environmental conditions might exacerbate discomfort. Developing coping mechanisms and strategies to avoid these triggers can significantly improve quality of life.
Importance of Proper Foot Care
Maintaining meticulous foot care is paramount for individuals with neuropathy. This involves regular, thorough inspection of the feet for any sores, cuts, blisters, or changes in skin color or texture. Early detection of potential problems allows for prompt treatment and prevents complications.
Proper footwear selection is also critical. Avoid tight-fitting shoes and those with high heels that can put additional pressure on the feet. Choose supportive shoes with good cushioning and adequate space for toes. Regular foot soaks, gentle exfoliation, and moisturizing can also be beneficial in maintaining foot health.
Physical Therapy and Exercise
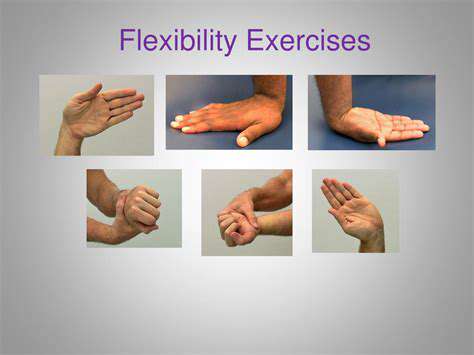
Physical therapy plays a crucial role in managing neuropathy-related issues in the feet. Exercises and stretches can help improve blood circulation, strengthen muscles, and enhance overall foot function. A physical therapist can develop a personalized exercise program tailored to the individual's specific needs and limitations.
Regular exercise, even low-impact activities like walking, can be beneficial for improving circulation and reducing pain. Consult with a healthcare professional before starting any new exercise routine to ensure it's safe and appropriate for your condition.
Nutritional Considerations
A healthy diet rich in essential nutrients can support nerve health and overall well-being. Including foods rich in vitamins B1, B6, and B12, as well as foods rich in antioxidants, can contribute to nerve function and reduce the risk of complications. A balanced diet, coupled with regular monitoring and management of underlying health conditions, can contribute significantly to managing neuropathy.
Seeking Support and Professional Guidance
Managing neuropathy requires a multi-faceted approach that includes professional guidance and support. Regular check-ups with a healthcare provider are essential for monitoring the progression of the condition, adjusting treatment plans, and addressing any emerging concerns. Joining support groups or connecting with other individuals facing similar challenges can provide invaluable emotional support and practical advice.
Open communication with healthcare professionals, family members, and support networks is vital for effective management. Understanding the specific needs and challenges associated with neuropathy can empower individuals to develop strategies that promote optimal well-being and quality of life.
Read more about Managing Neuropathy in the Feet
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health