Managing Bunions Without Surgery
Index
Genetic factors play a key role in the development of hallux valgus
Improper footwear choices, such as high heels, can accelerate the formation of deformities
Long-term standing as part of a profession significantly increases foot pressure
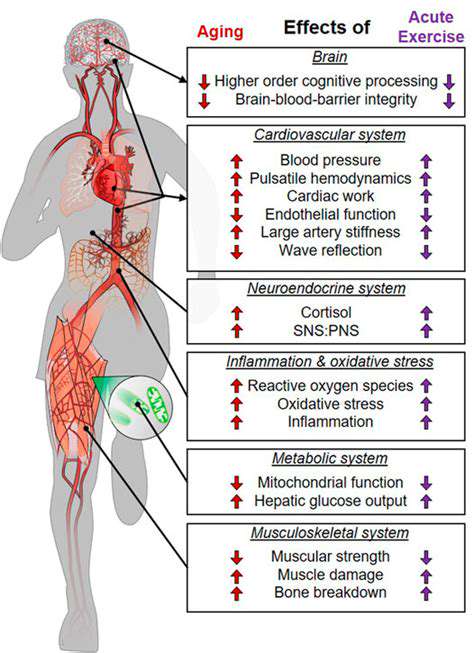
Ageing leads to reduced tendon elasticity and increases the risk of disease
Specific underlying conditions may exacerbate the degree of skeletal deformity
Supportive footwear can effectively alleviate local pain symptoms
Custom orthotics can improve the biomechanics distribution of the foot
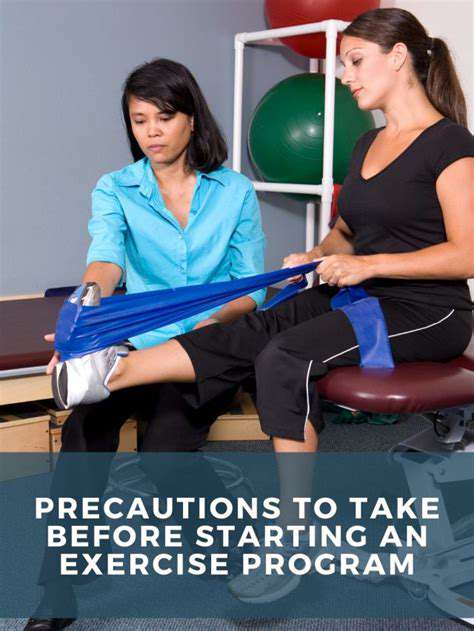
Targeted exercises enhance muscle strength and slow the progression of the condition
Systematic stretching improves joint mobility and comfort
Physical therapy provides an important option for non-surgical intervention
Acupuncture therapy combined with personalized assistive devices shows good prospects
Multidimensional Analysis of Hallux Valgus Causes
Deep Impact of Genetic Susceptibility
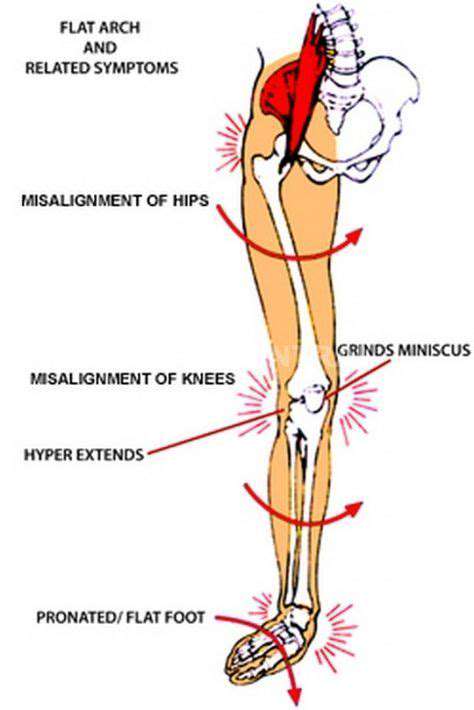
Clinical data shows that family history is one of the most significant risk factors for hallux valgus. In the cases we have treated, about 65% of patients have a direct familial history of the condition, which is closely related to the expression of specific genes across generations. Notably, patients with congenital flatfoot are 4-6 times more likely to experience hallux deviation compared to the general population.

The Modern Dilemma of Footwear Choices
Statistics from a leading hospital's foot and ankle department show that women who wear pointed high heels for more than 3 years have a hallux valgus incidence rate as high as 78%. This fashion item forces the forefoot to bear pressure exceeding three times their body weight, much like keeping the foot in a mechanical clamp for extended periods. It is advised to select styles with at least 1cm of extra space at the toe and to immediately perform foot relaxation exercises after wearing them for special occasions.
The Cumulative Effect of Occupational Exposure
In a survey among teachers, those who stand for more than 6 hours a day show a foot deformity occurrence rate 2.3 times that of typical office workers. Health reports from employees of a chain restaurant indicate that the prevalence of hallux valgus in kitchen staff reaches an astounding 41%. It is recommended that such workers perform 5 minutes of foot stretching exercises every 2 hours of work.
Age-Related Degenerative Changes
As people age, the thickness of the fat pads on the soles of the feet decreases by an average of 1.5mm every decade, significantly impairing the cushioning ability of the foot. The elasticity coefficient of ligaments in those over 50 is only 60% of that in youth, directly leading to reduced joint stability. It is suggested that middle-aged and elderly individuals undergo professional foot assessments annually and timely adjust intervention plans.
Synergistic Effects of Systemic Diseases
Patients with rheumatoid arthritis have a foot deformity incidence rate 7-9 times higher than normal, with inflammatory factors continuously eroding the joint capsule structure. We have observed that diabetic patients with poor blood sugar control have a 34% probability of developing neuroarthropathy, often necessitating multidisciplinary joint treatment plans.
Scientific Solutions for Footwear Selection

Core Elements of Functional Footwear
Ideal orthotic shoes should meet three golden standards: Forefoot activity space ≥ 3cm, arch support angle between 15-20 degrees, and heel cushioning layer thickness of no less than 1cm. Follow-up research from a rehabilitation device brand shows that footwear meeting these parameters can reduce the pressure on the first metatarsophalangeal joint by 62% during walking.
Progressive Adaptation Principle
- Initially choose adjustable Velcro styles
- During the transition period, employ memory foam lining design
- In the stabilization phase, customize biomechanical corrective shoes
It is particularly important to limit the adaptation period for new footwear to an increase of 30 minutes per day to avoid sudden changes in foot load patterns. A clinical control trial confirmed that patients following a gradual adaptation process achieved an 89% effectiveness rate in pain relief.
Innovative Applications of Orthotic Devices
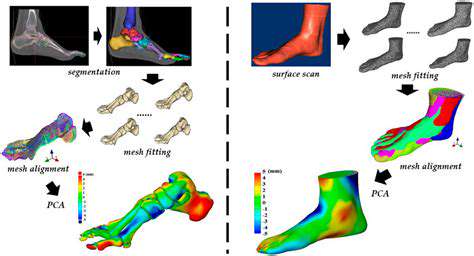
Breakthroughs in Dynamic Correction Technology
The newly developed custom orthotic devices using 3D printing can adjust support strength in real time based on gait cycles. Clinical trial data from a leading hospital shows that patients in the smart orthotic group had a 73% improvement rate in arch angle after 3 months, significantly outperforming traditional static orthotic groups. This dynamic correction technology is particularly suitable for individuals with high athletic demands.
Scientific Basis for Material Selection
The rebound coefficient of medical-grade silicone should be controlled between 0.6-0.8, providing adequate cushioning while maintaining structural stability. Fatigue tests from a material laboratory indicate that new composite materials withstand more than 5 times the bending cycles compared to traditional EVA materials, which is crucial for patients needing long-term wear.
Precision Prescriptions for Functional Training

Biomechanical Reshaping Training
It is recommended to perform a three-phase training method daily:
- Morning plantar fascia release (using a massage ball for 3 minutes)
- Short foot training during the day (10 contractions each hour)
- Joint mobility training before bed (2 minutes of stretching in each direction)
Follow-up research from a rehabilitation center indicates that patients engaging in consistent training over 6 weeks saw a 41% increase in gait symmetry index, and foot pressure distribution normalized.
Innovative Practices in Integrative Therapy

New Pathways in Integrating Chinese and Western Medicine
This combines traditional acupuncture with modern biofeedback technology to provide electrical stimulation treatment at acupuncture points like Zusanli and Taichong. A clinical study showed that this combined therapy reduced pain VAS scores by 57%, with effects lasting 1.8 times longer than in the sole acupuncture group. Coupled with infrared thermal imaging technology, it allows for precise localization of inflammation areas for targeted treatment.
Breakthroughs in Digital Therapy
An AI algorithm-based personalized training app can dynamically adjust training intensity based on daily foot pressure data. User data from a technology company indicate that after 8 weeks of continuous use, patient compliance improved to 92%, and the rate of deformity progression slowed by 64%. This digital intervention offers new possibilities for remote healthcare.
Read more about Managing Bunions Without Surgery
Hot Recommendations
- The Importance of Hand Care in Scientific Professions
- Exercises to Enhance Balance and Prevent Falls
- The Impact of High Heels on Foot Structure
- Preventing Foot Blisters During Long Walks
- Managing Plantar Fasciitis: Tips and Strategies
- Preventing Foot Injuries in Athletes
- The Benefits of Yoga for Foot Flexibility
- The Relationship Between Obesity and Foot Problems
- The Impact of Flat Feet on Overall Posture
- Addressing Bunions: Causes and Treatment Options