Common Fractures in the Hand and Arm
Arm fractures may affect the humerus, radius, or ulna. Humerus fractures can significantly impair shoulder and arm mobility. Prompt medical evaluation is essential to determine appropriate treatment, which might involve casting or surgery for complex cases.
Forearm fractures (radius/ulna) vary in location and displacement. The specific fracture characteristics dictate treatment, ranging from casts to surgical stabilization. These injuries often cause substantial pain and functional limitations.
Specific Considerations for Fracture Healing
Healing rates depend on age, health status, and fracture type. Nutritional support and strict adherence to treatment protocols significantly enhance recovery outcomes. Timely medical care and proper follow-up help ensure correct healing and minimize complications.
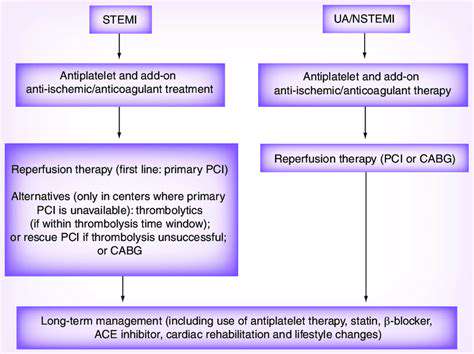
Diagnosis and Treatment Approaches
Diagnosis typically involves physical exams and imaging (X-rays or CT scans). Imaging choice depends on suspected fracture complexity and location. Treatment ranges from immobilization for simple fractures to surgical fixation for severe cases, with physical therapy playing a crucial role in rehabilitation.
Causes of Hand and Arm Fractures
Direct Impact
Direct blows from sports, accidents, or falls commonly cause fractures. Impact force determines fracture severity, with contact sports and workplace accidents being frequent culprits. Falls from height significantly increase fracture risk, emphasizing the importance of protective measures.
Indirect Force
Twisting or bending forces can fracture bones distant from the impact site. A classic example is wrist fractures from falls on outstretched hands, demonstrating how indirect mechanisms differ from direct trauma.
Repetitive Stress
Activities like baseball pitching or weightlifting can cause stress fractures through repeated microtrauma. These hairline cracks develop gradually, highlighting the need for proper training progression and rest periods.
Osteoporosis
This bone-weakening condition increases fracture risk from minor stresses. Postmenopausal women are particularly susceptible, requiring proactive management through medication and lifestyle adjustments.
Trauma from Sports or Physical Activity
While beneficial for health, sports involving collisions or repetitive motions elevate fracture risk. Sport-specific protective strategies are essential for injury prevention.
Underlying Medical Conditions
Conditions like osteogenesis imperfecta or rheumatoid arthritis compromise bone integrity, necessitating specialized care to prevent fractures.
Inadequate Calcium and Vitamin D
Nutritional deficiencies weaken bones over time. A diet rich in calcium and vitamin D, possibly supplemented with medical guidance, helps maintain skeletal strength.

Recovery and Rehabilitation
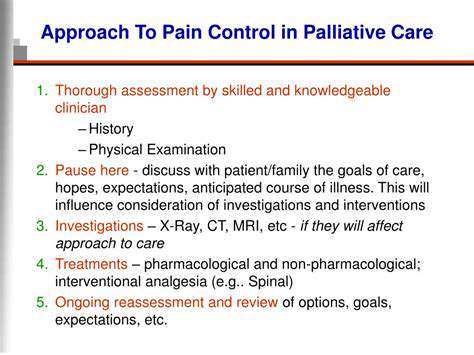
Pre-Rehabilitation Phase
This critical initial stage focuses on protecting the injury while initiating healing. Healthcare teams monitor immobilization and provide pain management strategies, setting the foundation for successful rehabilitation.
Immobilization and Pain Management
Proper casting or bracing ensures correct bone alignment during healing. Effective pain control enhances patient comfort and compliance with treatment protocols.
Range of Motion Exercises
Therapists carefully introduce movements to prevent stiffness once healing permits. These controlled exercises progressively restore joint mobility without compromising recovery.
Strengthening Exercises
As healing progresses, targeted exercises rebuild muscle strength and dexterity. Gradual progression is key to avoiding re-injury while restoring functional capacity.
Functional Restoration
Therapy shifts to task-specific activities mirroring daily needs, from fine motor skills to grip strength, ensuring practical recovery for real-world function.
Addressing Potential Complications
Vigilant monitoring catches issues like stiffness or nerve damage early, allowing timely intervention to optimize outcomes.
Return to Activity and Long-Term Management
A structured return to normal activities prevents overloading healing tissues. Ongoing guidance helps maintain gains and prevent future injuries through proper technique and conditioning.