Diagnosing Hand and Wrist Injuries
Recognizing the Signs and Symptoms of Common Hand and Wrist Injuries
Recognizing Sprains and Strains
Sprains and strains are common hand and wrist injuries often caused by sudden movements or forces exceeding the joint's capacity. A sprain involves damage to ligaments, the tough bands of tissue connecting bones, resulting in pain, swelling, and instability at the affected joint. Symptoms can range from mild discomfort to significant pain, making it difficult to move the injured area. Identifying the specific ligament involved, and the severity of the damage, is crucial for proper diagnosis and treatment. Immediate rest, ice, compression, and elevation (RICE) are often recommended as initial first aid measures to help manage pain and inflammation.
Strains, on the other hand, involve damage to muscles or tendons, the fibrous cords that connect muscles to bones. Strains typically manifest with pain, tenderness, and a reduced range of motion. The pain may be sharp or dull, and often worsens with movement. The location and characteristics of the pain can help differentiate between a sprain and a strain, but a proper diagnosis requires professional medical evaluation. Accurate diagnosis can help determine the best course of treatment, which might involve physical therapy, pain management, or rest.
Identifying Fractures
Fractures, breaks in the bones of the hand or wrist, are often characterized by severe pain, especially with movement. The pain may be localized to a specific area, or it may radiate throughout the hand or wrist. Visible deformity, such as a noticeable bend or displacement of the affected bone, is a common sign. Swelling and bruising are also frequently present. In addition to pain, patients might experience numbness or tingling in the fingers or hand, or experience weakness in the affected area.
Depending on the severity and location of the fracture, symptoms can vary. A small, hairline fracture might only cause mild discomfort, while a complete fracture can result in significant pain and difficulty with daily activities. If you suspect a fracture, seeking immediate medical attention is crucial for proper diagnosis and treatment. This is especially important to prevent further complications and ensure proper healing.
Assessing Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is a condition that results from compression of the median nerve in the carpal tunnel, a narrow passageway in the wrist. Common symptoms include numbness, tingling, and pain in the thumb, index, middle, and ring fingers. These symptoms are often worse at night or after periods of hand use. The pain may radiate up into the forearm, making it difficult to perform simple tasks like gripping or pinching.
Other symptoms of CTS can include weakness in the hand, making tasks like lifting or holding objects difficult. In more severe cases, individuals may experience a loss of grip strength. Recognizing these symptoms and seeking medical attention early can help prevent further complications and potential nerve damage.
Recognizing Tendonitis and De Quervain's Tenosynovitis
Tendonitis, inflammation of a tendon, can cause pain, tenderness, and stiffness in the affected area. The pain is often worse with movement and can be accompanied by swelling and warmth. Tendonitis typically affects the tendons in the wrist, hand, and fingers. It commonly develops from overuse or repetitive motions, such as typing, writing, or playing musical instruments.
De Quervain's tenosynovitis, a type of tendonitis, is characterized by inflammation of the tendons on the thumb side of the wrist. Symptoms often include pain and tenderness along the thumb-side of the wrist, and the pain may increase when moving the thumb or wrist. These conditions require proper diagnosis and treatment from a healthcare professional. Treatment options may vary based on the severity of the condition. Rest, ice, and over-the-counter pain relievers may be helpful for mild cases, while more severe cases may require physical therapy or other interventions.

Importance of a Thorough Medical History and Physical Examination
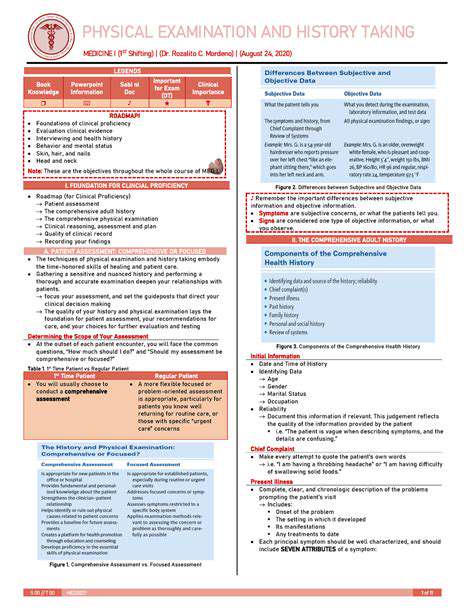
Comprehensive Medical History Taking
A thorough medical history is the cornerstone of effective patient care. It provides a detailed snapshot of the patient's health status, past experiences, and current condition. This crucial initial step allows healthcare providers to identify potential risk factors, understand the patient's perspective, and tailor treatment plans accordingly. Gathering a comprehensive medical history is not just a procedural formality; it's a fundamental aspect of patient-centered care, enabling a deeper understanding of the individual and their specific needs.
Accurate and complete medical histories are essential for developing accurate diagnoses and treatment plans. Incomplete or inaccurate information can lead to delayed or inappropriate interventions, potentially impacting patient outcomes. This detailed documentation helps track changes in the patient's health over time, facilitating proactive monitoring and early detection of potential complications. It also serves as a valuable reference point for future consultations and treatments.
Identifying Potential Risk Factors
A meticulous medical history allows healthcare professionals to identify potential risk factors for various illnesses and conditions. This includes past medical conditions, family history, lifestyle choices, and environmental exposures. By understanding these factors, healthcare providers can develop strategies to mitigate risks and promote preventative care, ultimately improving patient outcomes.
Analyzing the medical history for patterns and trends helps in early disease detection and intervention. This proactive approach is crucial for managing chronic conditions and preventing future complications. Recognizing predispositions or vulnerabilities enables the implementation of preventative measures, including lifestyle modifications, screenings, and vaccinations, to reduce the patient's risk profile.
Detailed family histories are often instrumental in identifying hereditary predispositions to certain diseases. This information allows for tailored screening and preventative measures to be implemented, potentially saving lives. A thorough understanding of the patient's medical history and family background can provide invaluable insights for proactive health management.
Tailoring Treatment Plans
A comprehensive medical history forms the basis for creating personalized treatment plans. Understanding the patient's specific needs, preferences, and health concerns allows healthcare providers to develop interventions that are tailored to the individual. This individualized approach ensures that treatments are not only effective but also align with the patient's values and lifestyle.
By incorporating the patient's perspective and experiences, treatment plans become more effective and better aligned with their goals. This personalized approach fosters patient engagement and adherence to the prescribed care. Ultimately, this leads to improved patient outcomes and a greater sense of empowerment in their own health journey.
Understanding past medical treatments, allergies, and medication responses allows healthcare providers to avoid potential complications and optimize treatment effectiveness. This nuanced understanding ensures that the chosen treatment plan is safe and aligns with the patient's overall well-being, minimizing adverse reactions and maximizing positive outcomes. Careful consideration of the patient's complete medical history is paramount for responsible and effective healthcare.
Read more about Diagnosing Hand and Wrist Injuries
Hot Recommendations
- The Impact of the Digital Age on Hand Function
- The Role of Hands in Agricultural Innovation
- The Impact of Technology on Hand Artistry
- The Importance of Hand Care for Artists
- How Hand Control Enhances Robotic Surgery
- The Impact of Hand Strength on Physical Labor
- How Handwriting Influences Cognitive Development
- The Impact of Environmental Factors on Hand Health
- The Power of Hands in Building Community
- The Importance of Ergonomics in Hand Health